Abstract







Source: https://www.sciencedirect.com/science/article/abs/pii/S0091743518301658?via%3Dihub

Promoting Good Practice In Prevention







Source: https://www.sciencedirect.com/science/article/abs/pii/S0091743518301658?via%3Dihub
by David Evans, Senior Counsel, CIVEL (USA)
January12, 2025
Article forwarded by Hershel Baker, Drug Free Australia. He opens by saying: “Please find evidence below on a current project to make the marijuana industry legally accountable to their victims in the U.S. if they are SUCCESSFUL, it will become very useful to Victims in many other countries including Australia.”
Legal Primer – Cannabis Industry Victims Educating Litigators (CIVEL) <https://www.civel.org/legalprimer>
The marijuana industry referred to here are those who illegally, negligently or fraudulently produce, market, or distribute marijuana products including those that have not been approved by the FDA or approved under federal law.
Today’s marijuana products can be high in potency and can reach 99% THC.
These products can be very destructive and cause addiction, mental illness, violence, crime, DUIs and many health and social problems. Young people are particularly vulnerable. We must protect them.
A first step is to educate lawyers and the community by providing legal and scientific guidelines for litigators so they can take the marijuana industry to court. We have produced six litigator guidelines:
We will arm the legal profession to recognize cases, prepare them and then litigate as was done in the cases against big tobacco and is now being done against the opiate companies.
We will not conduct litigation. Our goal is to get the legal profession to initiate litigation by educating them as to the legal issues and strategies involved. We also plan to educate the public about how the marijuana industry has destroyed lives and families and to support the victims.
For more information contact Senior Counsel, David G. Evans, Esq.
Email: seniorcounsel@civel.org <mailto:seniorcounsel@civel.org>
Please see our legal primer on marijuana and federal law
LEGAL PRIMER <https://www.civel.org/s/LEGALPRIMERCSA2017.pdf>
Other Important Documents
* CATEGORIES OF THE VICTIMS OF THE MARIJUANA INDUSTRY
<https://www.civel.org/list-of-marijuana-industry-victims>
* MARIJUANA AS A MEDICINE – POLICY, SIDE EFFECTS, SPECIFIC ILLNESSES
<https://www.civel.org/s/2CIVELMARIJUANA-AS-A-MEDICINE-POLICY-SIDE-EFFECTS-S
PECIFIC-ILLNESSES.pdf>
* THE FAILURES OF THE STATES TO REGULATE MARIJUANA
<https://www.civel.org/s/THE-FAILURES-OF-THE-STATES-TO-REGULATE-MARIJUANA-ST
UDIES-SHOW-THAT-MARIJUANA-PRODUCTS-HAVE-HIGH-LEVE.pdf>
* INTERACTIONS BETWEEN MARIJUANA AND OTHER DRUGS
<https://www.civel.org/s/4-CIVELINTERACTIONS-BETWEEN-MARIJUANA-AND-OTHER-DRU
GS.pdf>
* MARIJUANA AND VIOLENCE
<https://www.civel.org/s/5CIVELMARIJUANA-AND-VIOLENCE.pdf>
* MARIJUANA USE AND MENTAL ILLNESS AND BRAIN DAMAGE
<https://www.civel.org/s/6CIVELMARIJUANA-USE-AND-MENTAL-ILLNESS-AND-BRAIN-DA
MAGE.pdf>
* MARIJUANA USE AND DAMAGE TO HUMAN REPRODUCTION
<https://www.civel.org/s/7CIVEL-MARIJUANA-USE-AND-DAMAGE-TO-HUMAN-REPRODUCTI
ON.pdf>
* CONCERNS ABOUT CBD
<https://www.civel.org/s/8CIVEL-CONCERNS-ABOUT-CBD.pdf>
DISCLAIMER OF LEGAL ADVICE
This should not be considered legal advice. This is for informational purposes only. Use of and access to these materials does not in itself create an attorney – client relationship between David G. Evans or CIVEL and the user or reader. Mr. Evans or CIVEL cannot vouch for any study cited herein since they did not do the study. The readers should consult the study and make their own interpretation as to its accuracy. Please also be advised that case law and statutory and regulatory laws cited herein may have been amended or changed by the time you read this.
David G. Evans, Esq. – Senior Counsel – Cannabis Industry Victims Educating Litigators (CIVEL) (USA)
Source: Email by Herschel Baker <hmbaker1938@hotmail.com> Sent: 11 January 2025 23:06
Note by NDPA: This article describes harm Reduction as ” as an alternative to traditional abstinence-based education”. which is seen by NDPA as an unhelpful definition. The valid contribution of Harm Reduction can better be recognised as a strategy working in cooperation with Prevention i.e. it is case of applying ‘both’ rather than ‘either/or’.
One of the key findings from recent studies is the effectiveness of different types of interventions in educational settings. A scoping review identified various approaches, including cognitive-behavioral skill enhancement, peer interventions, and family-school cooperation, all of which have shown varying degrees of success in reducing substance use among adolescents[2]. Notably, while electronic interventions yielded mixed results, traditional methods like curriculum-based programs and peer support have been beneficial in addressing substance use issues[2].
Another significant study examined the long-term effects of a selective personality-targeted alcohol prevention program called PreVenture. This program was designed for adolescents exhibiting high-risk personality traits and demonstrated sustained positive outcomes in reducing alcohol-related harms over a seven-year follow-up period[3]. The findings suggest that targeted interventions can effectively delay the onset of alcohol use and mitigate its associated risks, highlighting the importance of tailoring programs to the specific needs of students.
Additionally, innovative approaches such as hybrid digital programs that combine e-learning with in-person sessions have shown promise. A study evaluating this method found significant reductions in substance use and increases in health knowledge among middle school students[5]. This approach addresses common barriers to implementation, such as limited class time and inconsistent delivery, making it a viable option for schools looking to enhance their substance abuse prevention efforts.
Furthermore, harm reduction strategies have gained attention as an alternative to traditional abstinence-based education. A pilot study on a harm reduction curriculum revealed significant improvements in students’ knowledge and behaviors related to substance use, suggesting that engaging students with relevant and relatable content can lead to better outcomes[4]. This approach challenges the conventional views on substance education and emphasizes the need for programs that resonate with adolescents’ real-life experiences.
Substance Abuse: The harmful or hazardous use of psychoactive substances, including alcohol and illicit drugs, leading to significant adverse consequences.
Cognitive-Behavioral Skills: Techniques that help individuals recognize and change negative thought patterns and behaviors associated with substance use.
Harm Reduction: A set of practical strategies aimed at reducing the negative consequences associated with substance use, rather than focusing solely on abstinence.
by William P. Barr & John P. Walters – 23 Jan 2025 | Hudson Institute
(This article forwarded to NDPA by Drug Free Australia)
Just weeks after the election, President-elect Trump announced that he would
impose a 25% tariff on all Mexican products, and an additional 10% tariff on
all Chinese products, until the flow of illegal narcotics from those
countries is stopped. These measures will do more to choke off the growing
scourge of illegal drugs than all steps taken in the “drug war” to date.
Over the past few years, the flow of illegal narcotics into our country has
become a tsunami, with seizures of fentanyl pills skyrocketing from 4
million in 2020 to 115 million last year. The devastation inflicted on
American society by this traffic is catastrophic.
The opioid crisis alone costs us over 100,000 overdose deaths and $1.5
trillion annually, while the flood of potent methamphetamine from Mexico
fuels a new wave of meth addiction, ravaging lives, families and
neighborhoods in its wake.
This deadly traffic happens by weakening our border defenses and ignoring
opportunities to choke off the supply chain for illicit drugs, now centered
in China and Mexico.
The U.S. policy has focused on “harm reduction” inside the U.S. – deploying
overdose medications, like Naxolone, and funding more treatment for
addiction. While these steps are unobjectionable in themselves, they are an
inadequate response to the flood of poison we are confronting. It is like
addressing violent crime by offering more bandages.
Real progress requires eliminating the drug supply at its source. Here the
U.S. has a golden opportunity because the supply chain for drugs poisoning
America has become highly concentrated and vulnerable. It depends entirely
on illegal activities in two countries – the manufacture of illicit drugs in
Communist China, and drug processing and distribution operations in the
cartels’ safe havens in Mexico.
All these illegal activities are carried out with – and indeed require – the
connivance or willful blindness of the host governments. As Trump’s
announced tariffs show, the U.S. has the tools and leverage to compel China
and Mexico to shut down these operations. Doing this would strike a decisive
blow: once these operations are dismantled, it would be impossible to
replicate them elsewhere at anywhere near their current scale.
China has become the hub of illegal drug production because illegal
narcotics are increasingly synthesized chemically, rather than made from
grown plants. China offers the two prerequisites needed to supply the U.S.
market: a large chemical industrial base, and a government willing to allow
its factories to make illegal narcotics and their precursors on a large
scale.
Chinese factories make the essential ingredients for virtually all the
fentanyl and other synthetic opioids, as well as 80% of the methamphetamine,
that come into the U.S. and are producing a new wave of drugs worse than
fentanyl, like nitazenes and xylazines (“tranq”). Simply put, without
China’s production, America’s drug problem would be mere fraction of what it
is.
Communist China could easily stop this activity if it wanted to. But a
recent report by the bipartisan Select Committee on the Chinese Communist
Party (CCP) shows that China’s participation in the illegal drug trade is a
deliberate policy.
According to the report, the Chinese government and the CCP has been
granting tax subsidies to encourage their drug companies to produce and
export – for consumption in the U.S. – fentanyl and other death-dealing
drugs that are illegal in China, the U.S. and throughout the world.
This is an intolerable situation. The U.S. must compel China to stop
producing these drugs by imposing an escalating series of consequences on
those involved.
The initial tariff announced by Trump is a critical first step. If it
doesn’t get results, further tools are available – imposing higher tariffs;
targeting sanctions against the Chinese drug companies involved, and
potentially indicting and seizing assets of those companies; sanctioning
Chinese banks found to be involved in laundering drug money; and
facilitating private lawsuits by fentanyl victims against Chinese companies
making the drugs.
The second major chokepoint in the drug supply chain lies in Mexico. The
Mexican cartels have become the “one-stop-shop” for processing and
distributing nearly all the illegal drugs coming into the U.S. – the
synthetic drugs made in China, as well as the cocaine from coca plants in
Latin America. Experience eliminating the Colombian Medellin and Cali
cartels in the early 1990s shows that the U.S. can dismantle these
organizations when it becomes directly involved, works jointly with the host
governments and local forces, and uses all available national security and
law enforcement tools.
But Mexico poses a particular challenge. Using bribery and terrorist
tactics, the cartels have cowed and co-opted the government to the point
that it is unwilling to confront them nor allow the U.S. to take effective
action against them. And, even if the Mexican government was willing to
tackle the cartels, their military and law enforcement is so rife with
corruption they are incapable of effective action by themselves.
Our country cannot tolerate a failed narco-state on our border flooding
America with poison. The only way forward is for the U.S. to use its massive
economic leverage to compel the Mexican government to take a stand against
the cartels. President Trump’s announced tariff does just this.
Because the Mexicans cannot do the job themselves, eliminating the cartels
will require a joint campaign through which the U.S. engages in direct
action against the cartels, using a range of our law enforcement,
intelligence and military capabilities. The Mexican cartels are more like
foreign terrorist groups, like ISIS, than they are the American mafia – and
it is heartening that President Trump has signed an executive order
designating them as such. It is time to confront them as national-security
threats, not a law-enforcement matter.
Attacking the source of the problem overseas does not mean we should pull
back from trying to dismantle trafficking operations inside the U.S. But
progress abroad will produce exponentially greater results than anything we
do at home. Trump’s tariff initiative shows, that, rather than dither with
America’s stubborn drug crisis and passing it on to his successor, Trump is
willing to tackle it head on with decisive action.
Source: https://drugfree.org.au/index.php
This is a response from Pamela McColl by email to the then BMJ editor-in-chief Dr Fiona Godlee to the article Drugs should be legalised, regulated and taxed
Every nation state, representing billions of individuals, on this planet opposes your view on the legalization of all drugs- aside from Uruguay who has in small measures legalized marijuana – with the misguided and pot using Prime Minister of Canada setting his own country up for the same fall sometime in 2018.
Nations who support the UN drug conventions and The Rights of the Child Treaty, spend on drug prevention and education, have the lowest rates in the world. Those who dabble in Sorosian drug ideology loose out and pay the price with populations suffering the impact of these harmful substances.
I have one simple question for you in light of your decision to focus on legal aspects of harm versus a serious consideration of health harms. Those who say the worst consequences of using marijuana are the penalties that can be imposed by the legal system is factually incorrect – unless the death penalty is included which I do not agree with nor does the United Nations and the drug preventions.
FACT: The legal ramifications are vastly over-rated including incarceration compared to the damage to an individual that can follow use.
Would you as a parent prefer to have your young adult child receive a ticket or intervention involving government agencies or law enforcement or even spend a couple of days in jail or would you prefer to see these drugs legalized – providing greater access, acceptability and normalization, and promotion by an addiction-for-profit industry ?
You need to compare the consequences of the use of marijuana that can be imposed on an individual with the risks of harm to body, and brain, including testicular cancer, a 7x fold increased risk of suicide, and significant increased risk of death by driving drugged – something 50% of users admit to doing ?
Is being charged with simple possession and serving a day or two in jail or being placed on probation or a handed a ticket in your view as harsh an experience and detrimental to an individual as living through a marijuana induced psychotic break from reality that may or not excite violence towards yourself or others?
Health rules the day and if the judicial penalties need to be addressed so be it – that is no reason to legalize a drug that is so dangerous to human health. There is every reason to educate the public on the vast array of marijuana harms and the harms other illicit substances pose.
Health Canada has this to say about the use of marijuana for any reason – including a medical reason. This information is being ignored by the Canadian government. We are about to repeat the thalidomide mistake once again, and all because a group of rogue bureaucrats and unenlightened politicians rule this day.
Cannabis should not be used if you:
Talk to your health care practitioner if you have any of these conditions. There may be other conditions where this product should not be used, but which are unknown due to limited scientific information.
Pamela McColl
http://www.preventdontpromote.org /;
Vancouver BC Canada
Source: Email from Pamela McColl May 2018
Roughly one in every three Americans have reported knowing someone who has died of a drug overdose, a new survey found.
The poll, conducted by researchers at Johns Hopkins Bloomberg School of Public Health, found that 32 percent of people have known someone who has died of a drug overdose. Those who reported knowing someone who has passed away from drug use were also more likely to support policy aimed at curbing addition, per the poll.
The survey results, published Friday in JAMA Network, suggest that an avenue for enacting greater policy change for addiction may be by mobilizing those who lost someone due to drug addiction, researchers wrote.
Experts also noted that opioids — often prescribed by doctors for pain management — especially with the proliferation of powerful synthetic drugs like fentanyl and polysubstance, have accelerated the rising rate of overdose deaths in recent years.
Since 1999, more than 1 million people have died of a drug overdose in the United States and while studies are still being conducted on the reasoning, researchers noted that there’s not much known about the impacts on the family or friends of the deceased.
The survey also found that personal overdose loss was more prevalent among groups with lower incomes but did not differ much across political parties.
Nearly 30 percent of Democrats said they lost someone to overdose, while 33 percent of Republicans and 34 percent of independents said the same.
“This cross-sectional study found that 32% of US adults reporting knowing someone who died of a drug overdose and that personal overdose loss was associated with greater odds of endorsing addiction as an important policy issue,” the researchers wrote. “The findings suggest that mobilization of this group may be an avenue to facilitate greater policy change.”
A similar study examined overdose deaths from 2011 to 2021 and estimates that more than 321,000 children in the U.S. have lost a parent to drug overdose.
According to the Centers for Disease Control and Prevention (CDC), U.S. drug overdose deaths dropped slightly in 2023, the first annual decrease in overdose deaths since 2018. Still, the overall number of deaths is extremely high, with more than 107,000 people dying in 2023 due to the overuse of drugs.
Source: https://www.msn.com/en-us/health/medical/nearly-1-in-3-americans-have-reported-losing-someone-to-a-drug-overdose-study/ar-BB1nsfVP?
ATLANTA — A new study led by a Georgia State University researcher finds that the opioid epidemic and rural homelessness are exacerbating each other with devastating consequences.
School of Public Health Assistant Professor April Ballard and her colleagues examined data from the Rural Opioid Initiative on more than 3,000 people who use drugs in eight rural areas across 10 states. They found that 54 percent of study participants reported experiencing homelessness in the past six months, a figure that suggests Point in Time Counts used to allocate state and federal funding significantly underestimate homeless populations in rural areas. The findings appear in the January edition of the journal Drug and Alcohol Dependence.
“Rural houselessness is very much an issue in the United States, and there are unique challenges that come with it, such as lack of awareness and a lack of resources,” said Ballard, who co-leads GSU’s Center on Health and Homelessness. “When you add the opioid epidemic on top of it, it really exacerbates the problem.”
Ballard explained that the unemployment, financial ruin and loss of family and social networks that often accompany opioid use disorder and injection drug use can precipitate housing instability and homelessness. The uncertain and harsh living conditions experienced by people without stable housing can perpetuate drug use as a coping mechanism. The result can be a self-reinforcing cycle that contributes to poorer health and shorter lifespans.
Ballard and her colleagues found that study subjects with unstable housing were 1.3 times more likely to report being hospitalized for a serious bacterial infection and 1.5 times more likely to overdose than those with stable housing. She explained that a lack of access to clean water to wash the skin and prepare drugs makes infections more likely, and that using drugs alone and furtively can increase the risk of an accidental overdose.
The Rural Opioid Initiative surveyed people about their experiences with homelessness over the past six months, while Point in Time Counts mandated by the federal Department of Housing and Urban Development quantify the number of people experiencing homelessness on a single night in January. Despite this methodological difference, Ballard said her study’s findings suggest that Point in Time Counts significantly underestimate homeless populations in rural areas.
In Kentucky, for example, the researchers counted up to five times as many people experiencing homelessness than Point in Time Counts, even though their sample of people who use drugs constituted less than 1 percent of the adult population. In three counties that estimated zero people experiencing homelessness using Point in Time Counts, Ballard and her colleagues quantified more than 100 people who use drugs who had experienced homelessness in the past six months.
The dispersed nature of rural areas makes Point in Time Counts difficult, Ballard acknowledged, but the undercounting of people experiencing homelessness can result in fewer federal and state resources reaching vulnerable people and communities.
“House-lessness in rural areas is a major problem,” Ballard said, “but we’re not allocating resources in a way that is proportionate to the problem.”
The research was supported by the National Institute on Drug Abuse with co-funding from the Centers for Disease Control and Prevention, Substance Abuse and Mental Health Services Administration, and the Appalachian Regional Commission.
Source: https://news.gsu.edu/2025/01/13/study-examines-links-between-opioid-epidemic-and-rural-homelessness/
Most Mondays, the Sixth Street entertainment district would be quietly nursing the hangover from another rowdy weekend, the only souls on the street those who sleep in the shelters, alleys, and sidewalks. But emergency dispatchers were getting repeated reports of people in distress.
The first call came in just after 9 a.m. from someone calmly describing an overdose in an alley. But, as the minutes dragged on, panic crept into the caller’s voice. “I’m scared,” she blurted out. “Oh, my gosh, I’m so fucking scared. Somebody’s going to die because of these people.”
“What happened?” asked the operator.
“Somebody tried to say ‘Don’t call the ambulance,’” the caller responded. “Oh, my God. Oh, my God.”
A little before 10 a.m., a security guard flagged down one of the Austin police officers flooding the district. Two men were sitting on the ground next to a trash bin in an alley near Sixth and Red River Street, slumped forward. Only 20 minutes earlier, both men had been walking and chatting. Now, they weren’t breathing.
The officer administered naloxone and began performing CPR. Paramedics took one to a hospital. The other, 51-year-old Benjamin Arzo Gordon, couldn’t be revived.
The alley where Gordon died had become the epicenter of a mass casualty event. During a two-hour span that Monday morning, at least six others overdosed and were revived with naloxone in a four-block radius in downtown Austin. Over 72 hours, Austin police reported more than 70 overdose calls. Records from Travis County, which includes most of Austin, and neighboring Williamson County indicate that as many as 12 may have died. The culprit: a bad batch of crack cocaine.
Through dozens of open records requests and interviews, the Texas Observer and Texas Community Health News have pieced together what happened during those deadly days—and how changes to state law might have saved lives. Across the capital city, people who consume crack, a stimulant, were suffering symptoms consistent with poisoning from opioids like heroin or fentanyl, the incredibly potent prescription painkiller.
The adulterated crack impacted Central Texans from many walks of life. Among the people who died were a construction worker from Honduras and a young man from Wimberley, who passed away in his parked truck with the engine running. Crack rocks found at the scene of some of the deaths tested positive for fentanyl.
A small, inexpensive item might have averted some of these deaths. Fentanyl testing strips can be used to check for the presence of the synthetic opioid. With an appearance similar to an at-home COVID-19 test, the strips are dipped in water in which a small amount of the drug has been dissolved. A line indicates if fentanyl is present.
But such testing strips are illegal in Texas. They’re considered paraphernalia, and possessing one is a Class C misdemeanor. While the Texas House passed a bill that would have legalized them in 2023, the Senate declined to vote on it.
In general, Texas has been reluctant to embrace the strategy of harm reduction, a broadly defined term for helping people who use drugs without stigmatizing or imposing strict parameters, while also involving drug users in planning and implementation. Harm reduction has been promoted in the United States since at least the 1980s. A classic early example is teaching people who inject drugs to clean needles with bleach, preventing the spread of HIV. The overall approach is sometimes pitched as a means to keep people alive long enough to get off drugs, but many practitioners simply seek to keep substance users safe and healthy, regardless of plans to enter treatment.
Under the administration of President Joe Biden, the federal government embraced aspects of harm reduction. Some states have as well. But policies favored by many Texas officials reflect the singular goal of making it as difficult as possible to use drugs. As it turns out, research and interviews with both experts and users of drugs show, making drug use more difficult also makes it more dangerous. Though Texas ranks low among states in fatal overdose rates, federal data shows the Lone Star State’s rate stayed nearly flat from 2023 to 2024, while overdose deaths fell significantly nationwide.
In recent months, top Texas officials have not only rejected harm reduction but have also openly antagonized those who practice it.
The prevailing attitude in the state is, “Why should we try and save their lives? They’re just going to use again,” said Joy Rucker, a nationally known advocate who launched Texas’ largest harm reduction nonprofit. In California, where she used to work, harm reduction organizations get robust public funding and operate openly.
“Texas was just a rude awakening,” she said.
A tall, thin Houston native with a quick sense of humor, Benjamin Arzo Gordon had been living on the streets of Austin for years. A January 2024 photo in the Austin American-Statesman shows him with a close-cropped white beard and a gray beanie, at Central Presbyterian Church downtown, looking pensive as he discusses harsh winter weather.
Andi Brauer, who oversees the church’s homeless outreach programs, said Gordon was a regular at weekly free breakfasts, cracking jokes with her and other volunteers and taking a genuine interest in her wellbeing.
“He’d always say, ‘You need to sit down and eat,’” Brauer recalled. “Or, if somebody was sometimes threatening or rude to me, he would say, ‘Don’t mess with Andi.’” She once printed out a photo of the two of them and used it to make a card for him.
In the alley where he died, Gordon was known to stop by with meals from the nearby food truck where he worked. “He used to help people in the alley,” said Loretta, a 55-year-old Austinite who herself suffered an overdose after Gordon.
Bokhee Chun, a Central Presbyterian volunteer, remembered Gordon would sing her hymns. Some months before he passed, Brauer said, Gordon came in to fill out a volunteer application.
Like many who died last April, Gordon was an experienced drug user. His drug of choice, crack, put him at little risk of sudden death by itself. But the crack he smoked that spring day was laced with a substance that has become synonymous with America’s failed drug policies.
Initially, fentanyl was used alone or to boost the potency of other opioids and depressants like heroin and prescription pain pills. But, in recent years, people killed by fentanyl are increasingly found to have stimulants like cocaine or methamphetamine in their systems. Explanations for this vary. Stimulants may be intentionally adulterated to hook users on fentanyl. A stimulant user might take opioids to come down. An unsophisticated dealer with a small stimulant supply may add fentanyl to stretch it. And failure to clean scales or surfaces can also mix fentanyl with another drug.
In Texas, overdose rates increased dramatically starting in 2020. From June 2023 to June 2024, more than 5,000 people died of an overdose in the state, with Travis County recording the highest fentanyl-related death rate among Texas’ most populous counties in recent years. Though Texas has one of the lower overdose rates in the nation, deaths in the state declined by less than 3 percent from 2023 to 2024, while the rest of the nation saw a drop of nearly 15 percent, per the federal Centers for Disease Control and Prevention. In October, the Texas Department of Health and Human Services (HHS) announced that it recorded a 13-percent drop in the state over the same period—but its figures include only those overdoses deemed accidental, not those labeled intentional, suicide, or of undetermined cause.
Experts also question the general accuracy of Texas’ numbers. In much of the state, underfunded and under-trained justices of the peace are charged with death investigations. Overdoses, which require costly autopsies and toxicology reports, are easy to overlook.
In response to the overdose increase, HHS in 2017 launched the Texas Targeted Opioid Response (TTOR) initiative. HHS is also part of a state awareness campaign using billboards and social media ads focused on cautionary tales of young Texans who overdosed. At the same time, state leaders have doubled down on criminalization.
In 2023, the Legislature passed a law allowing prosecutors to bring murder charges in fentanyl overdose cases. Critics say this discourages people from reporting emergencies, and research shows such laws harm public health. Some who overdosed in Austin last April had shared drugs, putting survivors at risk of being charged. In 2021, the Legislature passed a good samaritan law ostensibly meant to protect people who call 911 to report an overdose. The law created a defense for people arrested for low-level possession, but it has so many caveats—you can only use it once in your life, it doesn’t apply if you’ve been convicted of a drug-related felony, you can’t use it if you’ve reported another overdose in the last 18 months—that you’d need a flow chart to understand it. Critics say the statute’s of little use.
“The fentanyl-induced or the drug-induced homicide laws, that jacks up the consequences and the intensity so much more,” said Alex White, director of services at the Texas Harm Reduction Alliance, an Austin non-profit that does street outreach, operates a drop-in center, and provides supplies including for hygiene and wound care.
Some states, like Maryland and Vermont, make a point of prioritizing input from people who use or have used drugs while crafting policy. Harm reduction advocates say this is lacking in Texas, though HHS does have a low-profile advisory committee that is required to include members who’ve received mental health or addiction treatment.
“If you’re thinking that you know how to serve folks, and you don’t have those folks at the table when you’re trying to serve them, it’s not going to work,” said Stephen Murray, a paramedic and overdose survivor on Massachusetts’ Harm Reduction Advisory Council.
Rapid changes in the drug supply can make it difficult to conclusively track policy impacts. Critics blame Texas’ persistent overdose rate at least partly on punitive laws, but a few western states including liberal Oregon—which famously passed a drug decriminalization ballot measure in 2020—actually saw overdoses increase between 2023 and 2024. To this, some experts and at least one study counter that fentanyl’s delayed arrival on the West Coast has distorted the death rates, and that Oregon specifically did not implement sufficient services alongside decriminalization.
Texas Governor Greg Abbott’s office did not respond to a request for comment for this story.
Loretta woke up on the morning of Monday, April 29, in the alley where she often goes to smoke crack and sometimes spends the night. She grew up in East Austin, only blocks away.
Loretta said she lent her pipe that morning to a friend who’d just purchased drugs. Then she heard someone ask, “What’s wrong?” and saw the friend staring up, trance-like.
“He stayed looking at the sky,” Loretta said, reclining and rolling back her eyes to demonstrate. “The next thing I know he just went like this,” she said, as she pantomimed slumping limply to the side. “I was shaking him, and I said, ‘What’s wrong, what’s wrong?’ And after that he just didn’t answer.”
Despite fear she’d be held responsible, Loretta yelled to a friend to call 911. Police and paramedics swarmed the area. Loretta watched as someone else collapsed. “She hurt herself hard on the concrete and I said, ‘Oh, my God, hell no, this is not happening.’”
Soon, an acquaintance ran up to say Loretta’s boyfriend had also collapsed in a nearby portable toilet. “He was slurring like a baby, like a little boy,” Loretta said. “He started to lose consciousness. I slapped him hard. It hurt my hand. And I shook him and I started praying.”
Around the time that Loretta was calling out for help for her boyfriend, and EMTs were trying unsuccessfully to save Gordon, Adam Balboa showed up to work at an Austin-Travis County EMS (ATCEMS) station in south Austin. A case manager for a unit focused on substance use, Balboa heard the overdose reports and symptoms being described and knew what would save the most lives. “We needed to flood the downtown area with as much Narcan as possible,” he said.
Opioids in the bloodstream bind to receptors in the brain, creating euphoria. But by a quirk of physiology, excessive opioids bound to those receptors interfere with the body’s ability to measure its need for oxygen, slowing breathing—to the point where it can be fatal. Mouth-to-mouth resuscitation can keep someone alive. Narcan temporarily blocks the receptors to opioids, essentially short-circuiting an overdose if delivered in time.
The medics and police officers in downtown Austin were running out of naloxone, but Balboa didn’t just want to get them more. He also wanted to get it in the hands of people who use drugs, along with their friends, family, and neighbors. So he and colleagues began throwing together kits containing Narcan, a CPR mask, and instructions, and he hurried downtown with his SUV loaded up with the blue zippered pouches. “Everybody was super receptive,” he said. “They were clipping it to their belts and … going about their normal business.”
As common-sense as that response seems, it’s one strongly associated with harm reduction. By handing out naloxone downtown, Balboa was helping those most vulnerable to the tainted drugs help one another. It’s also a response that would have been impossible a few years ago.
Balboa’s unit is the brainchild of Mike Sasser, a 51-year-old ATCEMS captain who’s been in recovery for 21 years. A longtime paramedic who often worked with Austin’s unhoused population, Sasser became friends in 2018 with Mark Kinzly, a lion of the Texas harm reduction movement. Kinzly, who passed away in 2022, had helped start the Texas Overdose Naloxone Initiative, which was getting grants to distribute the medication. He had a seemingly simple idea for Sasser: ATCEMS could use grant money to buy Narcan, pass it out, and train people how to use it.
“My mind was blown,” Sasser said. “Why have I never thought about this? That would save so many lives.”
ATCEMS doctors then wrote prescriptions that allowed medics to hand out naloxone (today, it’s available over the counter). Sasser’s unit also began reaching out directly to overdose survivors and administering a maintenance drug that reduces opioid cravings, and it now includes two full-time case managers who run an overdose reversal education program called Breathe Now.
All of this fits under the philosophy of harm reduction, which can also include teaching people to use drugs more safely and providing supplies like clean glass pipes, which help prevent disease and infection. Providing food, water, hygiene products, or wound care to people who feel stigmatized in doctor’s offices is another tenet.
“We want to provide people with what they need, so we can build that trust,” said Em Gray, whose NICE Project provides supplies to Austinites, many of them unhoused, and stocks Narcan vending machines. “That’s how we show that we are there for them; we’re there to improve their quality of life, there to reduce their overdose death rates.”
There’s little funding available in Texas for the nonprofits and mutual aid groups that do this work. Across the state, harm reductionists often operate out of backpacks or car trunks.
To the state’s credit, Texas has taken some steps to increase naloxone distribution. TTOR does this with an annual federal grant of about $5.5 million. In 2019, TTOR, whose Narcan distribution program is administered by the University of Texas Health Science Center at San Antonio, gave about 40 percent of its naloxone to law enforcement agencies—even as research shows it’s more effective to give the medication to laypeople, who are typically first on the scene and present no threat of arrest—an analysis by Texas Community Health News found. By 2022, TTOR’s emphasis had shifted, with law enforcement making up only about 15 percent of its distribution.
But police are still prioritized in Texas’ long-term naloxone plan. Under a different state program started in April 2023, the Texas Department of Emergency Management (TDEM) began distributing $75 million worth of the medication over 10 years. That naloxone, donated by a pharmaceutical company as part of a court settlement over opioid deaths, is largely earmarked for first responders. Of the more than 150,000 doses that TDEM distributed from April 2023 to September 2024, 118,000 went to law enforcement agencies, mostly sheriff’s offices. Many of these offices cover areas that lack other harm reduction infrastructure, but records provided by TDEM show sheriffs aren’t using the naloxone. Of 13 counties in which agencies reported using doses from TDEM by September, the highest rate of use was 3 percent. Much of that naloxone will expire later this year. In an email, a TDEM spokesperson said the agency had “yet to turn down a request for naloxone” and that “Administration or disposition of distributed naloxone is up to the receiving entity how they see fit, in accordance with manufacturer’s guidance.”
When it set the state’s two-year budget in 2023, the Legislature allocated an additional $18 million in opioid settlement funds to UT Health San Antonio, but it’s not clear the appropriation will be renewed.
In the meantime, harm reductionists rely on a patchwork of naloxone sources, including local governments.
“Had we not saturated Austin with Narcan leading up to [the April] event, then that event would have been a lot more detrimental than it was,” said Sarah Cheatham, a peer support specialist with The Other Ones Foundation, an Austin nonprofit serving the unhoused. “Even when it was hard to get in our hands, we were out there doing this communication for months before this happened.”
By late morning on April 29, the Austin Police Department (APD) had some idea what was happening. Crack rocks and pipes had been found at the scene of a number of overdoses in an area known for its use, and officers had interviewed some who’d been revived with naloxone. They began looking for people seen on surveillance cameras and suspected of selling the tainted crack. While responding to an overdose, detectives found one suspect standing in front of a tent, just a block from police headquarters.
While cops made arrests, harm reductionists tried frantically to figure out what was going on. A little after noon that Monday, Claire Zagorski, a graduate research assistant at the University of Texas at Austin who’s worked in harm reduction for years, messaged a group chat: “Austin folks there’s a bad batch downtown as of this AM. Not sure on specifics but it does respond to naloxone.”
Groups started handing out Narcan and warning the communities they serve, but without any official information from local governments. “We were really just kind of going in blind,” Cheatham said. “We were all talking to each other about, ‘Who’s going to these camps? Where is it happening? Is it happening downtown?’ And I was mainly reaching out to the people that I know.”
Research shows that, given the chance, drug users will reduce their risk of overdose—including by carrying naloxone, not using alone, or taking a small tester dose. But, lacking detailed information, harm reduction workers in Austin were constrained. “It’s distressing that the thing that got everyone activated was me being notified by a backchannel,” Zagorski said.
When local officials finally made public statements hours after the flood of 911 calls, they only addressed some questions. Whatever was killing people was responding to Narcan, officials said, in a news release and press conference. But they were vague about which drug was adulterated, and there was no mention of test strips.
“It was a very chaotic scene at first,” APD Lieutenant Patrick Eastlick told the Observer. “Something we can look at in the future is, if this happens again, that we reach out to these different groups where we can spread the word.”
Open conversations about drugs are difficult in a state where top elected officials are cracking down on services for people who use them. In late November, state Attorney General Ken Paxton filed a headline-grabbing lawsuit to shut down a homeless navigation center at a south Austin church. The suit specifically blames the Texas Harm Reduction Alliance’s needle exchange program for “the prevalence of drug paraphernalia, including used needles, littering the surrounding area.” Drug use around the church “fuels criminality, and creates an environment where nearby homes and businesses are at constant risk of theft,” the complaint states.
Critics say efforts like Paxton’s just push drug use out of sight, creating greater risk. “It sends the message to people who use drugs that they should hide it, they should be kept in the dark and in the closet,” said Aaron Ferguson of the Texas Drug User Health Union. “The closet is a very dangerous place for people who use drugs. It’s where overdoses happen. It’s where stadiums full of people die every year.”
At least two who died in the Austin overdose outbreak were found alone. Family members of at least two others who perished at home told police they didn’t know their loved one had used drugs that day.
How state officials talk about drug use, critics note, also suggests that only some lives matter. For example, in a 2023 legislative hearing, GOP state Senator Drew Springer—in a successful attempt to woo conservative support for requiring school districts to stock naloxone in middle and high schools—distinguished between different groups of Texas children. “I think the general public, when they hear ‘overdosing,’ they think ‘That’s just a druggie, and that’s a druggie kid’s problem,’” he said. “No, it’s your kid’s [problem], because he may be taking a Xanax or an Adderall” without knowing fentanyl was present.
Claudia Dambra, who runs Street Value, a drug user health organization in Houston, criticized messaging that condemns certain substance users. “All it’s doing is creating more separation,” she said. “It feels like this weird, forced social Darwinism. … It feels like they’re picking us off.”
In an email, an HHS spokesperson said the agency does not discriminate: “[HHS] substance use programs offer treatment and recovery support for people, regardless of substance use duration.”After the horror of watching her boyfriend taken away in an ambulance, Loretta wandered through downtown Austin. Near APD HQ, in the area where police had arrested their suspect earlier, she was offered crack that her friend insisted came from a reliable source. Stressed and scared, she took a hit.
“I started getting a headache right away, like oh, my God, I’ve got a migraine or something. And I started throwing up,” she said. “I said, ‘Call the police, I’m sick.’”
Loretta didn’t lose consciousness, but she was vomiting as police questioned her. Eventually, she was taken to a hospital. She would be among the survivors.
Today, Loretta says that she gets test strips from harm reduction organizations, which quietly distribute them despite state law, and she gives them to friends. But, at the time, she knew little about them. Organizations that distribute strips generally can’t use grant money for their purchase, and government agencies, like ATCEMS, don’t distribute them.
Back in 2023, it seemed Texas was poised to legalize the strips. Before that year’s legislative session, Abbott said he supported allowing the tests, and legislators in both chambers introduced bills to legalize equipment for checking a range of drugs. One by Houston-area Republican Tom Oliverson, which was limited to fentanyl strips only, sailed through the House.
Oliverson, an anesthesiologist who has prescribed fentanyl to patients, said he’d heard from family members of people who purchased black-market pills without knowing they included the powerful opioid.
“That’s literally like stepping on a landmine,” Oliverson told the Observer. “You heard a click and the next thing you know, you were gone. Nothing you could have done could have saved you. You didn’t know it was there, right? Except for the fact that there are test strips.”
The bill received tepid support from harm reductionists, who were frustrated by its narrowness. The drug supply is constantly changing: Today, the dangerous veterinary tranquilizer xylazine is increasingly used to supplement other drugs. “We’re really trying to craft language that’s inclusive,” said Cate Graziani, former head of the Texas Harm Reduction Alliance and current co-director of a spinoff advocacy group, Vocal TX. “We don’t want to go back to the Legislature every time we have a new overdose prevention tool.”
Oliverson said the bill only applied to fentanyl “because it is that much more dangerous, because it is that much more powerful. … People say to me, ‘I don’t like the idea of giving people test strips because it gives them confidence in the illegal drugs that they’re buying, and I want to discourage people from using illegal drugs,’” he said. “Well, I want to discourage people from using illegal drugs too, but having them insta-killed by a mislabeled pill that they bought, the first time they took it, is not an effective strategy for recovery.”
While other drug-checking legislation failed that session, Oliverson’s bill passed the House 143-2—but it never received a hearing in the Senate Criminal Justice Committee. “They just could not get over the idea that you are making it safer for people to use illegal drugs and that we shouldn’t make it safe for people to use illegal drugs,” Oliverson said, “because they shouldn’t be using illegal drugs at all.”
Oliverson said he’ll introduce a similar bill this session and may rewrite it to include xylazine, but he made it clear he doesn’t support other harm reduction measures like needle exchanges. Such a bill will simply fizzle again, though, barring a change of heart in the Senate, which is run with an iron fist by Republican Lieutenant Governor Dan Patrick, whose office did not respond to arequest for comment for this article.
“It’s so demoralizing to live in a state where your elected leadership is so unwilling to do something so small as legalizing fentanyl test strips, because there’s so much stigma around drug users,” Graziani said.
By the afternoon of April 29, the tainted crack had made its way to south Austin. Loretta Mooney, another ATCEMS case manager in the substance use unit, was off work but rushed in. Dispatchers could see a new cluster of calls developing on Oltorf Street, east of Interstate 35.
By the time Mooney responded to her first call, at an apartment complex, medics had administered naloxone and revived a woman. Mooney handed out a few doses, then responded to another call from a fast food restaurant across the street. Someone had flagged down police, concerned about a man collapsed against the restaurant’s wall. Officers began CPR and administered Narcan. Mooney gave the man an additional dose and continued life-saving measures. Still, the 53-year-old died.
The situation was starting to look similar to downtown earlier in the day. Teenagers at another apartment complex began waving down Mooney and the officer. They ran over. Mooney administered naloxone to an unconscious woman and helped the officer deploy a breathing bag and mask. After a few minutes, the woman began breathing on her own again.
With Balboa now on his way to meet her and most of the calls near her covered, Mooney came to the same conclusion Balboa had that morning. “I was like, ‘Bring me all the Narcan you have and we’re going to start teaching these kids,’” she said.
On the lower level of a terraced parking lot, Mooney and the officer spread out naloxone kits and gathered the teenagers who had flagged them down.
“I’m telling the kid that came to get me specifically … ‘Because of you, this woman is alive,’” Mooney said. “We’re on the side of [the road] with, you know, ages 10 to 16, teaching them how to use Narcan.”
While Mooney and then Balboa, too, instructed people in the neighborhood how to use naloxone, a new crisis emerged. Some of the people who had bought the tainted crack were now behind the wheel. First responders were rushing to car wrecks and stalled vehicles.
Responding to the new calls, Mooney and Balboa saw the results of their impromptu training. As Balboa headed to a pawn shop where someone was overdosing, he got stopped in traffic. With his lights and sirens going, trying to weave through vehicles, he saw the teenagers they’d trained earlier.
“Before I can clear an intersection, they’d already sprinted over, pulled out a kit, and started giving Narcan,” he said. “Not only were they excited and ready to help and empowered to be able to do so, but when that opportunity finally came for them, they ran at it.”
As evening fell, the dying slowed. Behind closed doors, away from passersby armed with naloxone, however, it wasn’t through yet. A woman staying at a motel on Oltorf woke up during the night and called her 61-year-old husband, only to hear his phone ringing in the bathroom, then find him lying on the floor. The partner of a 57-year-old man got out of bed to get him warm milk after she noticed his nose bleeding, but, when she came back, he wasn’t breathing. A 36-year-old parked his truck in a lot in north Austin; when a security guard called 911 hours later, he was already dead. Around midnight, a son found his 63-year-old father deceased in an Oltorf apartment.
Later that same Tuesday, Loretta was released from the hospital. Downtown again, she found out her boyfriend had also survived and been released.
The following day, a man in southeast Austin woke up in the afternoon to find that a friend he’d let stay in his apartment had died while he slept. After agonizing for nearly two hours, he called the cops. That afternoon, a 34-year-old resident of Williamson County, just north of Austin, was found on the floor of his bedroom, where police found crack laced with fentanyl. Between April 28 and May 6, nine people in Travis County died from the toxic effects of fentanyl and cocaine, according to Travis County Medical Examiner records, in addition to the Williamson County death. At the request of APD, the Travis medical examiner withheld the cause of death in two other fatal overdoses that may have been related.
In the aftermath, APD made a handful of arrests. In some cases, police affidavits show, detectives were following information about who may have sold the tainted crack; in others, undercover officers simply went to known drug markets and arrested anyone who would sell to them. Eastlick, the APD lieutenant, said investigators believe the crack was adulterated at the local level, not higher up the drug supply chain, but that police had been unable to prove anyone intentionally sold tainted drugs. “It was a short surge … so our thinking is that it was not intentional,” he said.
As the tainted substance faded from the Austin drug supply, Cheatham said she and others heard stories of people who overdosed and were revived by naloxone without the authorities ever being alerted. In Austin’s camps and alleys, anonymous drug users helped one another.
Many of those who died remained anonymous as well, victims of an event whose details remained unclear and which took its toll mostly on the sort of people society tends to lose in its cracks.
Brauer and Chun, with the Central Presbyterian church, didn’t learn of Benjamin Arzo Gordon’s death until months afterward, when contacted for this story. In early November, the pair traveled to the indigent burial cemetery in northeast Travis County. In the wide, level graveyard, rows of nondescript markers rested flush to the ground. By Gordon’s, they left a bouquet of artificial flowers and a potted plastic plant.
“Just being able to picture him so clearly, knowing him as somebody that I value, that I enjoyed seeing, that was full of life and laughter despite the situation he was in—to hear about the way that he died of a drug overdose, probably fairly anonymously, just was incredibly sad to me,” Brauer said. “So because I didn’t get a chance to say goodbye … it just felt like something we needed to do to honor him.”
Editor’s Note: This article was produced in collaboration with Texas Community Health News and Public Health Watch. Daniel Carter contributed reporting.
Source: https://www.texasstandard.org/stories/texas-war-on-drug-users-fentanyl-overdoses-narcan-austin/
by Charles Hymas Home Affairs Editor 14 January 2025 Telegraph, London
Watchdog warns weapons and phones are being delivered to inmates with the devices, posing a threat to national security
HMP Manchester is among the prisons that have allowed basic security to fall into disrepair making it easier for gangs to access the grounds.
Drone-flying drug gangs have seized control of prison airspace in a move that threatens national security, a watchdog has warned.
Charlie Taylor, the chief inspector of prisons, said the service had “in effect ceded the airspace” to two high-security category A jails, allowing organised crime gangs to deliver drugs, phones and weapons to inmates who included organised crime bosses and terrorists.
He said HMP Long Lartin, in Worcestershire, and HMP Manchester had thriving illicit economies of drugs, mobile phones and weapons because basic security measures such as protective netting and CCTV had been allowed to fall into disrepair.
At Manchester, almost four in 10 (39 per cent) of prisoners had tested positive in mandatory drug tests. Half of inmates at Long Lartin, one of Britain’s top security jails, told inspectors it was easy to get drugs and alcohol. Some 27.2 per cent had tested positive for drugs.
Long Lartin has housed some of Britain’s most notorious prisoners, including hate preachers Abu Qatada and Abu Hamza. Among those currently being there are Jordan McSweeney, the murderer of law graduate Zara Aleena, and serial killer Steve Wright, jailed for life for the murder of five women in Ipswich in 2016. Mr Taylor said violence and self-harm at both jails had increased, in part driven by drugs and the accompanying debt prisoners found themselves in.
There had been six self-inflicted deaths at Manchester since 2021, with a seventh taking place a few weeks after the inspectors’ visit.
At Long Lartin, violence had increased by about 50 per cent since the last inspection in 2022. It was higher than at other category A jails, with more than 200 assaults on staff or prisoners in the last year. Forty per cent of prisoners said they felt unsafe.
“It is highly alarming that the police and prison service have, in effect, ceded the airspace above two high-security prisons to organised crime gangs which are able to deliver contraband to jails holding extremely dangerous prisoners including some who have been designated as high-risk category A,” he said. “The safety of staff, prisoners and ultimately that of the public, is seriously compromised by the failure to tackle what has become a threat to national security.
“The prison service, the police and other security services must urgently confront organised gang activity and reduce the supply of drugs and other illicit items which so clearly undermine every aspect of prison life.”
Charlie Taylor said violence and self harm had increased inside the prisons in part due to the rise of drug use and associated debt.
The scale of the problem at HMP Manchester, previously known as Strangeways, included inmates burning holes in windows to receive drone deliveries which prompted Mr Taylor to last year tell the Justice Secretary to put the prison into emergency measures.
The latest warning comes after Mr Taylor likened high-security jail HMP Garth in Lancashire to an “airport” because there were so many drones flying in drugs.
A report from Independent Monitoring Boards (IMB) – made up of volunteers tasked by ministers with scrutinising conditions in custody – into “crumbling” jails in England and Wales said delays in fixing broken prison windows were making it easier for drones to be used to deliver drugs and weapons. In December, MPs heard contraband was being taken into HMP Parc in South Wales in “children’s nappies”, while there were “industrial specification drone drops being organised by organised crime gangs”.
Source: https://www.telegraph.co.uk/news/2025/01/14/drone-flying-drug-gangs-seize-control-of-prison-airspace/
Dr. Nora Volkow outlines a new roadmap for cannabis and cannabis policy research. In this uncertain and rapidly changing landscape, Dr. Volkow emphasizes that research on cannabis and cannabis policy is badly needed to guide individual and public health decision-making.
The greatly increased availability of cannabis over the last two decades has outpaced our understanding of the public-health impacts of the drug. It is now available for medical purposes in most states, and adults may now purchase it for recreational use in nearly half the states. With greater availability has come decreased public perception of harm, as well as increased use.
In this uncertain and rapidly changing landscape, research on cannabis and cannabis policy is badly needed to guide individual and public health decision-making.
The National Survey on Drug Use and Health reported that between 2012 and 2019, past-year use of cannabis among people 12 and older rose from 11 percent to over 17 percent, and although trend comparisons aren’t possible because of changes in the survey’s methodology, in 2022, nearly 22 percent of people had used the drug in the past year. Very steep increases are also being seen in the number of people 65 and older who use cannabis.
At the same time, the cannabis industry is producing an ever-wider array of products with varying and sometimes very high concentrations of delta-9-tetrahydrocannabinol (THC) Greater harms from cannabis use are associated with regular consumption of high-THC doses. And there is a cornucopia of other intoxicating products available to the public, some containing other cannabinoids about which we still know very little.
To create a roadmap for research in this space, NIDA along with the National Center for Complementary and Integrative Health (NCCIH), the National Cancer Institute (NCI), and the Centers for Disease Control and Prevention (CDC), sponsored an independent consensus study by the National Academies of Sciences, Engineering, and Medicine (NASEM). The study resulted in a comprehensive report, Public Health Consequences of Changes in the Cannabis Policy Landscape, that was published in September.
The report describes in detail the different regulatory frameworks that exist in different states, and it draws on prior research to identify policies that are likeliest to have the greatest impact protecting public health. Those include approaches like restrictions on retail sales, pricing, and marketing; putting limits or caps on THC content in products; and laws about cannabis-impaired driving. They also could include different forms of taxation and even state monopolies. While state monopolies have not yet been tried with cannabis, they have proven effective at reducing the public health impacts of alcohol.
But the report also underscores that few conclusions can yet be drawn about the impacts of legalization or the different ways it been implemented. It is clear that people are consuming cannabis more and in a wider variety of ways, and there is some evidence of increases in emergency department visits due to accidental ingestion, car accidents, psychotic reactions, and a condition of repeated and severe vomiting (hyperemesis syndrome). But we are hindered in our further understanding because policy details vary so much between states and because data are collected and reported in so many different ways, making interpretation difficult.
Consequently, the report enumerates recommendations for research that should be conducted by federal, state, and tribal agencies to provide greater clarity and inform policy, including several domains within the purview of the NIH.
The report underscores the need for more detailed information on health and safety outcomes associated with specific policy frameworks. This includes more data on outcomes associated with different regulations for how cannabis products are sold and marketed, whether they can be used in public spaces, and whether more restrictive rules about how cannabis can be sold, such as those existing in other countries like Uruguay, are associated with improved health and safety outcomes. Many states have developed approaches to promote health and social equity, including programs to expunge or seal records of cannabis offenses and preferential licensing for individuals or groups most adversely impacted by the disparities in criminal penalties, but whether these programs will achieve their intended goals also requires careful evaluation.
Finally, more research is needed on the health effects of cannabis use by specific groups like youth, pregnant women, older adults, and veterans, and on its effects in individuals with various medical conditions for which medicinal cannabis might be used. Studies are also needed on health effects of the high-potency and synthetic or semi-synthetic cannabinoid products that are emerging. But the authors underscore that the focus cannot solely be that of risks—it must also include research on potential benefits of cannabis in managing some chronic mental or physical health conditions as well as interactions with prescription drugs that patients may already be taking to manage their health issues.
Much of this research will require or benefit from better surveillance of cannabis cultivation, product sales, and patterns of use. Existing surveillance, as the report points out, has suffered from a lack of funding and coordination, producing gaps in our knowledge. There is also a need for better tests for detecting cannabis impairment. Unlike alcohol, THC remains in the body long after its psychoactive effects have worn off. So, unlike commonly used alcohol sobriety tests, blood tests for cannabis that are currently widely used in law enforcement and employment screening cannot distinguish between recent or past use. Better surveillance and improved tests can inform research on interventions to mitigate risks to health and safety associated with cannabis use. They can also help inform the development of cannabis product safety and quality standards.
Some of the pressing questions identified by the NASEM report are already research priority areas for NIDA. For instance, our medicinal cannabis registry, which was funded starting in 2023, will be able to inform research, policy, and practice by gathering longitudinal data about cannabis use and outcomes from a cohort of people using the drug medicinally. The project will include a program to test the composition and potency of cannabis products used and will integrate registry data with other data sources.
The NIDA-funded Monitoring the Future survey has tracked nationwide cannabis use trends in adolescents and young adults for decades. The survey has recently recorded reduction in teenage use of substances in general, including cannabis, and recent surveys have also shown increases in disapproval of cannabis use and perception of its harms in this age group. However, it continues to show that cannabis is one of the most-used drugs by teenagers, with a quarter of 12th graders reporting use in the past year.
Since its launch nearly a decade ago, the trans-NIH Adolescent Brain Cognitive Development (ABCD) study has been collecting longitudinal data on drug use and its developmental impacts in a large national cohort from late childhood through early adulthood. More recently, ABCD has been complemented by a similar study on the first decade of life, the multi-Institute Healthy Brain and Child Development (HBCD) study. HBCD is recruiting a cohort of pregnant participants across the country and will use neuroimaging and other tools to track the impacts of prenatal exposure to cannabis and other environmental influences on the developing brain. By identifying risk and resilience factors for cannabis use in youth, the data from ABCD and HBCD will be extremely valuable in informing prevention programs in these age groups.
Advances in cannabis and cannabis policy research could be aided by wider adoption of the standard 5mg unit of THC required in research studies funded by NIDA and other NIH Institutes. Adoption of this standard was based on the need for consistency across research studies, which will facilitate more real-world-relevant research and translation of findings into policy and clinical practice. Research using this standard could also provide better insights into the effects of cumulative exposure and long-term developmental and cognitive effects of prenatal exposure.
Scientific research should always drive best practices in public health. To that end, NIDA and other NIH institutes will continue to support essential research on cannabis, the health effects of new products, and the effects of policy changes around this drug. It is essential to ensure that, where they are legal, product contents are accurately represented to the consumer in an environment where public health takes precedence over profits.
Source: https://nida.nih.gov/about-nida/noras-blog/2025/01/new-roadmap-cannabis-cannabis-policy-research
Health-risk behaviors such as binge drinking, drug use, and violence are common among college students. These issues are especially prevalent among first-year students living away from their families for the first time. According to the American Addiction Centers, nearly half of all college students would qualify for at least one substance use disorder.
A pilot and feasibility study by Kenneth W. Griffin and colleagues found that using VR technology to prevent substance misuse and violence is both feasible and engaging. 100% of participants agreed that the program could be implemented on college campuses.
“VR for reducing adolescent risk behaviors is an emerging area of research, focusing mostly on developing VR modules that are appealing and feasible,” Griffin explains. “This study is novel in that it examines the viability of VR technology to provide virtual role-play and skills practice opportunities to supplement an existing evidence-based drug and violence prevention approach.”
VR has been shown to help treat mental health conditions like anxiety, phobias, and PTSD. Griffin and colleagues are testing whether this technology can effectively prevent substance misuse and violence.
In the pilot study, researchers developed a series of VR modules that put users in different virtual social situations. For example, participants might witness someone being drugged at a party or see a classmate cheating. In choosing the best response for each situation, they practice cognitive-behavioral skills for preventing risk behaviors with their virtual peers. These skills may include assertive communication, negotiation, compromise, conflict resolution, or bystander intervention strategies. The VR sessions supplemented online e-learning modules lessons based on the LifeSkills Training program.
Before and after the training, participants took the same assessment. Results showed improved decision-making and stronger anti-violence attitudes.
Due to the program’s success, the research team secured additional grant funding from the CDC’s National Center for Injury Prevention and Control. Griffin emphasizes the need for more research. “While VR may be a useful tool for reducing youth health risk behaviors, more rigorous controlled trials are needed to determine whether VR technologies can produce behavioral outcomes and the duration of these effects. The new funding will allow us to conduct a rigorous test of this innovative technology for preventing substance misuse and violence among university students.” Griffin says.
The study dovetails with the College of Public Health’s commitment to harnessing the power of immersive technologies to improve health and health education. The College is home to the Center for Immersive Technologies and Simulation. There, students are trained to use VR in nursing, social work, health administration, and public health. Griffin’s study was not conducted in this Center.
“Using virtual reality technology to prevent substance misuse and violence among university students: A pilot and feasibility study” was published in Health Informatics Journal in October 2024. The study was funded by the Centers for Disease Control and Prevention’s National Center for Injury Prevention and Control and developed in collaboration with National Health Promotion Associates (NHPA), a research and development company that developed and markets the LifeSkills Training program. Griffin, a former employee and current consultant with NHPA, worked closely with the team in this pilot and feasibility study of the VR modules.
Additional authors, all from NHPA, include: Gilbert J. Botvin, Weill Cornell Medical College; Christopher Williams, Purchase College, State University of New York; Sandra M. Sousa.
Source: https://publichealth.gmu.edu/news/2025-01/virtual-reality-pilot-program-shows-promise-preventing-substance-misuse-and-violence
According to the Health Ministry’s Survey on Drug Use in Secondary Education in Spain (ESTUDES 2023), the average at which young people begin to consume alcohol is 13.9 years of age; tobacco, 14.1; and cannabis, 14.9. One of the risk factors for substance use is the influence of those who are already using, and who share common characteristics, among young people’s social peers or equals, with these including classmates and others friends.
Not all young people, however, decide to take these substances, so the question arises of what factors protect an adolescent from using substances when others around them are. This question was also posed by Raquel Espejo Siles and Joaquín Rodríguez-Ruiz at the University of Cordoba’s Coexistence and Violence Prevention Studies Lab (LAECOVI), proving that, although there is a great variety of protective factors (including individual, family and school ones), there are, in fact, two aspects that should guide prevention policies: age and type of substance.
Espejo and Rodríguez-Ruiz confirmed this after a bibliographic analysis that began with more than 8,000 research articles, reduced to 50 after discarding those that did not meet the inclusion criteria set down in the systematic review. Based on all this scientific evidence, they concluded that age is essential, since an adolescent does not relate to substances in the same way at age 10 as they do at age 17, for example. Family or school factors, such as parental supervision and feelings of attachment to one’s school, protect against substance use in early adolescence, but they lose their influence and cease to do so as the years go by.
“As adolescence progresses and peers become more influential, prevention strategies should place more emphasis on peer culture. As of the age of 16, when their development is more advanced, they can address individual issues such as promoting self-control and responsible decision-making,” Rodríguez-Ruiz added.
Similarly, the type of substance must also be taken into account. According to all the studies analyzed, an individual factor like assertiveness is not effective against the separate consumption of alcohol, tobacco, or cannabis, but it does protect against polyconsumption.
In addition to taking into account the substance, and age, prevention strategies should also be updated taking into account vaping and the influence of social media. As Espejo Siles explains: “we are dealing with a changing phenomenon, with new forms of consumption and new ways in which adolescents relate to each other”.
Published in the journal Adolescent Research Review, the study also delves into the need for studies to unify their criteria (such as defining adolescence in the same way) and to expand their geographical diversity, since most are based on American culture.
Source: https://www.eurekalert.org/news-releases/1070392
Prevention is key, and we cannot forget that today’s marijuana is highly potent. In 2025 and beyond, federal agencies must prioritize public health and safety and work to undo legalization’s harmful consequences.
The Department of Health and Human Services (HHS) is positioned to implement a wide range of policy initiatives to prevent marijuana use and hold the industry accountable. For example, marijuana legalization has re-elevated the conversation about second-hand smoke. California recently passed a law permitting “cannabis cafes” in which users can openly smoke marijuana. Second-hand marijuana smoke has been found to be more harmful than second-hand tobacco smoke and contains many of the same cancer-causing substances. Our country has legally and culturally rejected indoor cigarette smoking. HHS must stand on science and reject indoor marijuana smoking by publishing strict guidelines prohibiting it, just as it did with indoor cigarette smoking.
Transparency within the “medical” marijuana industry is also desperately needed. As it did with opioids, HHS should create a registry of medical marijuana recommendation practices and make the information available to the public. The database could include information regarding regional breakdowns, a list of overprescribing doctors, and pot-industry kickbacks received by doctors.
Sunlight is the best disinfectant when it comes to quack doctors. In August, a Spotlight PA article uncovered Pennsylvania medical pot doctors who were doling out thousands of medical marijuana cards per year. These are similar to the “pill mills” that fueled the opioid epidemic.
Last year, the Food and Drug Administration (FDA) bucked federal legal precedent around marijuana rescheduling by inventing new, lower standards. Its flawed marijuana rescheduling review was designed to permit marijuana rescheduling. The ramifications of changing this precedent aren’t limited to marijuana; other dangerous drugs (e.g., psychedelics) could be reclassified to a lower schedule based on the new lax standards. HHS should issue internal agency guidance that advises FDA to adhere to the established five-factor test for determining currently accepted medical use. This will ensure that drug scheduling, which has direct implications for the availability of drugs, remains science based.
The Trump-Vance administration must soundly reject moving marijuana from Schedule I to Schedule III for one simple reason: marijuana fails to meet the legal definition of a Schedule III drug. It has not been approved by the FDA for the treatment of any disease or condition. Moving marijuana to Schedule III is a handout to corporations, as it would allow companies to deduct advertising and other expenses from their taxes, fueling the growth of an industry that profits from addiction.
Far from being a legitimate medicine, marijuana is harming the millions of Americans who misuse it. Given that 3 in 10 users develop a marijuana use disorder, better known as addiction to marijuana, the incoming administration needs to focus on helping connect Americans to treatment.
Federal law enforcement also plays a crucial role in curbing marijuana legalization and its effects. In 2013, the Obama administration issued the Cole Memo, a document that cemented the federal government’s non-enforcement policy on marijuana. The first Trump administration rescinded the memo, but more must be done to enforce federal laws already on the books. The Justice Department has the power to prevent distribution to minors, curtail drugged driving, and investigate state-legal dispensaries being used as a cover for illegal drug trafficking—all things the Obama administration promised to do. By beginning with this targeted enforcement strategy, law enforcement can shut down the operations of the industry’s worst actors.
To promote public safety, the Trump-Vance administration should also crack down on illegal marijuana grows, particularly those in remote areas on federal lands. These operations are often controlled by cartels and poison the surrounding natural environment with toxic chemicals.
We also need a new national anti-drug media campaign, updated for the 21st century. This campaign must broadcast messages widely through traditional and social media and talk about the dangers and truth behind the use of drugs. The Office of National Drug Control Policy (ONDCP), the drug policy office within the White House, has a key role to play, too, particularly in drug use prevention. ONDCP helps oversee the Drug-Free Communities Support Program, which is responsible for much of our federally funded drug prevention work. In an era in which drugs are sold and marketed via social media, it’s more important than ever that effective anti-drug prevention messages reach young people. ONDCP also oversees the High Intensity Drug Trafficking Areas program, which forms a crucial partnership between local, state, and federal law enforcement to curtail drug trafficking. Both these programs’ funding should be protected and prioritized.
A good strategy must focus on all drugs, but we can’t ignore the politically inconvenient ones. If President Trump wants to make America healthy again, the conversation must include marijuana, a drug with an addiction rate of up to 30 percent that is being pushed by a profit-driven industry that desperately needs federal accountability.
Dr. Kevin Sabet is the President of Smart Approaches to Marijuana (SAM) and the Foundation for Drug Policy Solutions (FDPS) and a former White House drug policy advisor to Presidents Obama, Bush and Clinton.
SOURCE: https://www.newsweek.com/making-america-healthy-again-must-start-better-drug-policy-opinion-2014657
Our 50th year brought hope, as we finally saw evidence of a sustained downturn in drug overdose deaths. From July 2023 to July 2024, the number of fatal overdoses dropped nearly 17 percent, from over 113,000 to 94,000. We still don’t know all the factors contributing to this reversal, so investigating the drivers of this decline will be crucial for sustaining and accelerating the downturn. We also need to recognize that the decline is not homogenous across populations: Black and American Indian/Alaskan Native persons continue to die at increased rates. And 94,000 people dying of overdose in a year is still 94,000 too many.
As we begin a new year, I see four major areas deserving special focus for our efforts: preventing drug use and addiction, preventing overdose, increasing access to effective addiction treatments, and leveraging new technologies to help advance substance use disorder (SUD) treatment and the science of drug use and addiction.
The brain undergoes continuous development from the prenatal period through young adulthood, and substance exposures and myriad other environmental exposures can influence that development. Prenatal drug exposure can lead to learning and behavioral difficulties and raise the risk of later substance use. Adverse childhood experiences, including neglect, abuse, and the impacts of poverty, as well as childhood mental disorders, can negatively impact brain development in ways that make an individual more vulnerable for drug use and addiction. Early drug experimentation in adolescence is also associated with greater risk of developing an SUD.
Early intervention in emerging psychiatric disorders as well as prevention interventions aimed at decreasing risk factors and enhancing protective factors can reduce initiation of drug use and improve a host of mental health outcomes. Research on prevention interventions has shown that mitigating the impact of socioeconomic disadvantage counteracts the effects of poverty on brain development,1 and some studies have even documented evidence of intergenerational benefits, improving outcomes for the children of the children who received the intervention.2 Studies have also shown them to be enormously cost-effective by reducing later costs to healthcare and other services, providing health and economic benefits to communities that put them in place.3
Yet, in the United States, efforts to prevent substance use have been largely fragmented, and the infrastructure and funding required to bring effective programs to scale is lacking. What kinds of policy innovations could we put into place to ensure that everyone who could benefit from evidence-based prevention services has access to them, whether through school, healthcare, justice, or community settings? NIDA, along with other NIH Institutes, the Centers for Disease Control and Prevention, and the Substance Abuse and Mental Health Services Administration, have charged the National Academy of Sciences, Engineering, and Medicine with creating an actionable blueprint for supporting the implementation of prevention interventions that promote behavioral health. The report is due out early this year and has the potential for tremendous public health impact.4
We also need to continue research toward mitigating fatal overdoses. Comprehensive data on overdose reversals do not currently exist, but recipients of SAMHSA State Opioid Response grants alone reported more than 92 thousand overdose reversals with naloxone in the year ending March 31, 2023, and this is likely just a small fraction of the lives saved. We do not yet know the extent to which greater use of naloxone has played a role in the recent declines in overdose fatalities, but this medication, the first intranasal formulation of which was developed by NIDA in partnership with Adapt Pharma, is a real public health success.
NIDA is supporting research to evaluate approaches to naloxone distribution, for instance through mobile vans and peer-run community services that also provide sterile injection equipment to prevent HIV and HCV transmission. We are also supporting research on new approaches to reversing drug overdoses, such as wearable devices that would auto-inject naloxone when an overdose is detected and electrical stimulation of the phrenic nerve to restore breathing, a method already used in resuscitation devices.5 We are also supporting research on compounds that could potentially reverse methamphetamine overdoses, such as monoclonal antibodies and molecules called sequestrants that bind and encapsulate methamphetamine in the body.6
In 2023, only 14.6 percent of people with an SUD received treatment, and only 18 percent of people with an opioid use disorder (OUD) received medication.7 Stigma, along with inadequate coverage of addiction treatment by both public and private insurers, contributes to this gap. To fix this will require partnering with payors to develop and evaluate new models for incentivizing the provision of evidence-based SUD care.
Increased access to methadone is a particularly high priority in the era of fentanyl and other potent synthetic opioids. Results from a recent study in British Columbia showed that risk of leaving treatment was lower for methadone than for buprenorphine. Risk of dying was similarly low for both groups.8 Currently in the United States, methadone is only available from specialized opioid treatment centers, but studies piloting access through pharmacies have shown promise.
OUD medications also need to be accessible to people with SUD in jails and prisons. Research conducted in justice settings has shown that providing access to all three FDA-approved medications for OUD during incarceration reduced fatal overdose risk after release by nearly 32 percent.9 Access to buprenorphine during incarceration was also associated with a 32 percent reduction in recidivism risk.10 Through NIDA’s Justice Community Overdose Innovation Network (JCOIN), we continue to promote research into innovative models and strategies for integrating medications for OUD in justice settings.
I am also hopeful that we will soon see increased utilization of contingency management for treating stimulant use disorders. Providing incentives for treatment participation and negative drug tests is the most effective treatment we have for methamphetamine and cocaine addictions, but implementation has been hindered by regulatory ambiguities around caps on the dollar value of those incentives. However, demonstration projects underway in four states (California, Washington, Montana, and Delaware) are implementing contingency management with higher incentives and could further bolster evidence for the effectiveness—including cost effectiveness—of this approach.
There are many promising new technologies that could transform the treatment of addiction, including central and peripheral neuromodulation approaches. Transcranial magnetic stimulation (TMS) was already approved by the FDA as an adjunct treatment for smoking cessation and peripheral auricular nerve stimulation was approved for the treatment of acute opioid withdrawal. TMS, transcranial direct current stimulation (tDCS), and peripheral vagal nerve stimulation are under investigation for treating other SUDs. Low-intensity focused ultrasound—a non-invasive method that can reach targets deep in the brain—is also showing promise for the treatment of SUD. NIDA is currently funding clinical trials to determine its safety and preliminary efficacy for treating cocaine use disorder11 and OUD with or without co-occurring pain.12
Advances in pharmacology have helped identify multiple new targets for treating addiction that are not limited to a specific SUDs like OUD. Instead, these targets aim to modulate brain circuits that are common across addictions; they include among many others D3 receptor partial agonists/antagonists, orexin antagonists and glucagon-like peptide 1 (GLP-1) agonists. The latter are particularly promising, as these types of drugs, including semaglutide and tirzepatide, are already being used for the treatment of diabetes and obesity.
Anecdotally, patients taking GLP-1 agonists report less interest in drinking, smoking, or consuming other drugs. Recent studies based on electronic health records have revealed that people with SUDs taking GLP-1 medications to treat their obesity or diabetes had improved outcomes associated with their addiction, such as reduced incidence and recurrence of alcohol use disorder,13 reduced health consequences of smoking,14 and reduced opioid overdose risk.15 NIDA is currently funding randomized clinical studies to assess the efficacy of GLP-1 agonists for the treatment of opioid and stimulant use disorders and for smoking cessation.
Creation of large data sources and repositories in parallel with advances in computation and analytical modeling including AI are helping in the design of new therapeutics based on the 3D molecular structure of addictive drugs and the receptors they interact with.16 NIDA-funded researchers have published studies showing that AI could be used to provide more timely, comprehensive data on overdose, such as by using social-media to predict overdose deaths.17 It could be used to enable higher-resolution analyses in basic neuroscience research18 and facilitate studies using large data sources like electronic health records.19 AI is also being used to support delivery of behavioral therapies and relapse prevention in virtual chatbots and is being studied in wearable devices. Although there is much work to be done to ensure that AI is deployed safely and ethically, particularly in clinical settings, this technology has considerable potential to enhance and expand access to care.
AI will also be transformative for analyzing big data sets like those being generated by the Adolescent Brain Cognitive DevelopmentSM (ABCD) Study and HEALthy Brain and Child Development Study. These landmark NIH-funded studies are gathering vast quantities of neuroimaging, biometric, psychometric, and other data across the first two decades of life. They will be able to answer important questions about the impacts of drugs and other environmental exposures on the developing brain, inform prevention and treatment interventions, and establish a valuable—and unprecedented—baseline of neurodevelopment that will be a crucial resource in pediatric neurology.
The field of addiction science has progressed at a breathtaking pace. These advances could not have been made without the commitment of an interconnected community of people. Researchers, clinicians, policymakers, community groups, and people living with SUDs and the families that support them all play a role in collaboratively finding solutions to some of the most challenging questions in substance use and addiction research. Together, we turn our eye to 2025 and the challenges and opportunities ahead.
 |
Contemporary issues on drugsAs well as providing an in-depth analysis of key developments and emerging trends in selected drug markets, the Contemporary issues on drugs booklet looks at several other developments of policy relevance. The booklet opens with a look at the 2022 Taliban ban on the cultivation and production of and trafficking in drugs in Afghanistan and its implications both within the country and in transit and destination markets elsewhere. This is followed by a chapter examining the convergence of drug trafficking and other activities and how they affect natural ecosystems and communities in the Golden Triangle in South-East Asia. The chapter also assesses the extent to which drug production and trafficking are linked with other illicit economies that challenge the rule of law and fuel conflict. Another chapter analyses how the dynamics of demand for and supply of synthetic drugs vary when the gender and age of market participants are considered. The booklet continues with an update on regulatory approaches to and the impact of legalization on the non-medical cannabis market in different countries, and a review of the enabling environment that provides broad access to the unsupervised, “quasi-therapeutic” and non-medical use of psychedelic substances. Finally, the booklet offers a multi-dimensional framework on the right to health in the context of drug use; these dimensions include availability, accessibility, acceptability, quality, non-discrimination, non-stigmatization and participation. |
Key findings and conclusionsThe Key findings and conclusions booklet provides an overview of selected findings from the analysis presented in the Drug market patterns and trends module and the thematic Contemporary issues on drugs booklet, while the Special points of interest fascicle offers a framework for the main takeaways and policy implications that can be drawn from those findings. |
Sources:
Issues: https://www.unodc.org/unodc/en/data-and-analysis/wdr2024-contemporary-issues.html
Findings and Conclusions: https://www.unodc.org/unodc/en/data-and-analysis/wdr2024-key-findings-conclusions.html
by DFAF.org
|
by Miles Martin – milesmartin@ucsd.edu –
A recent study analyzing data from the National Survey on Drug Use and Health (NSDUH) found that past-year recreational ketamine use among adults has increased dramatically since 2015, including significant shifts in associations with depression and sociodemographic characteristics such as race, age and education status. Ketamine use has shown promise in clinical trials therapy for several mental illnesses, including treatment-resistant depression, and the new research suggests that ongoing monitoring of recreational use trends is crucial to balancing these clinical benefits against the risk of unmonitored recreational use.
Key findings include:
The researchers recommend expanding prevention outreach to settings like colleges, where younger adults may be at heightened risk, as well as providing education on the harms of polydrug use, particularly in combination with opioids. As medical ketamine becomes more widely available, they also emphasize the need for continued surveillance of recreational ketamine use patterns and further research to understand the factors that contribute to ketamine use.
The study, published online in the Journal of Affective Disorders, was led by Kevin Yang, M.D., a third-year resident physician in the Department of Psychiatry at UC San Diego School of Medicine. The research was supported by the National Institute on Drug Abuse of the National Institutes of Health.
Source: https://today.ucsd.edu/story/ketamine-use-on-the-rise-in-u.s-adults-new-trends-emerge
Ketamine could be upgraded to a Class A drug as the government seeks expert advice on its classification, the Home Office has said.
Illegal use of the drug has reached record levels in recent years, with an estimated 269,000 people aged 16-59 reporting ketamine use in the year ending March 2024.
Increasing ketamine’s classification would bring it in line with drugs including cocaine, heroin and ecstasy (MDMA) and mean up to life in prison for supply and production.
The policing minister will ask the Advisory Council on the Misuse of Drugs whether its classification should be changed and “carefully consider” its findings.
Ketamine can cause serious health problems including irreversible damage to the bladder and kidneys.
It is also one of the most detected drugs in incidents of spiking.
While commonly used on animals and in healthcare settings, ketamine is also thought of as a party drug due to its hallucinogenic effects.
An estimated 299,000 people aged 16-59 reported ketamine use in the year ending March 2023 – the highest on record.
Ketamine was upgraded from a Class C substance in 2014 due to mounting evidence over its physical and psychological dangers.
Currently, the maximum penalty for producing and supplying ketamine is up to 14 years in prison. Possession can carry up to five years in prison, an unlimited fine, or both.
Should it be upgraded to a Class A drug, supply and production of it could carry up to life in prison,, external while possession could carry up to seven years in prison, an unlimited fine, or both.
A coroner’s prevention of future deaths report called for action over the drug’s classification, after a man died from sepsis caused by a kidney infection that was “a complication of long-term use of ketamine”.
Greater Manchester South senior coroner Alison Mutch noted that James Boland, 38, started taking the drug as he believed it to be “less harmful” than Class A drugs.
She wrote , externalin November: “Maintaining its classification as a Class B drug was likely to encourage others to start to use it or continue to use it under the false impression it is “safer”.”
Policing minister Dame Diana Johnson has pledged to “work across health, policing and wider public services to drive down drug use and stop those who profit from its supply.
“It is vital we are responding to all the latest evidence and advice to ensure people’s safety and we will carefully consider the ACMD’s recommendations before making any decision.”
Irish teenagers whose friends use cannabis are 10 times more likely to consume the drug themselves, according to the findings of new research.
It also highlighted how teenagers who felt it was necessary to use cannabis to fit in with their friends were almost twice as likely to use the drug compared to those who did not feel peer pressure to use cannabis.
Teenagers who believed their parents would be ambivalent towards their use of cannabis were also almost four times more likely to be current users of the drug than those students who thought their parents were strongly against cannabis use.
The findings are based on the responses by over 4,400 students in fourth and fifth year to a questionnaire issued as part of the Planet Youth survey carried out in late 2021.
The respondents were based across 40 schools in north Dublin, Cavan and Monaghan.
The study highlighted how current cannabis users among such an age group were significantly more likely to also be consuming alcohol, smoking or vaping.
It also reveals that low parental supervision was significantly associated with higher odds of current cannabis use.
The authors of the study, whose findings are published in the Irish Journal of Psychological Medicine, said its rationale was to examine individual, familial, peer, school and community factors associated with cannabis use by adolescents in Ireland in order to provide measures for prevention and early intervention.
They claimed several of the risk factors identified by the research have the potential to be modified through drug prevention strategies.
The researchers noted that earlier studies had found that long-term use of cannabis has the potential to lead to addiction with one in three regular adolescent users becoming addicted to the drug, while also having the potential to exacerbate mental health issues such as psychosis.
The study observed that cannabis-related psychiatric admissions for people aged 15-34 in the Republic rose by 140 per cent between 2011 and 2017 and have remained at the same elevated level ever since.
Despite the evidence of increased health risks associated with cannabis use, the study said adolescents continue to use cannabis for a number of various factors including boredom relief, appetite increase, sleep improvements and increased social opportunities.
Other factors can include low self-esteem and insecurity or family problems.
Asked to assess their own mental health, almost three-quarters of the teenagers (72.4 per cent) who do not use cannabis said it was good or OK compared to 54.6 per cent among cannabis users.
In contrast, 45.0 per cent of cannabis users assessed their mental health as bad or very bad compared to 27.1 per cent of those who do not use the drug.
Similarly, only 16.6 per cent of cannabis users perceived the drug to be harmful, while 67.2 per cent of non-users surveyed believed it could have a negative impact on their health.
Among cannabis users, 90.4 per cent reported that their friends also use the drug compared to 29.3 per cent of students who do not use it.
One of the report’s main authors, Teresa O’Dowd, said they believed it was the first study in an Irish setting which found no significant difference in cannabis use between males and females.
Dr O’Dowd, a specialist in public health medicine with HSE North West, said the lack of association between gender and cannabis use was a notable finding as historically male gender had been noted as a risk factor for use of the drug.
She said the finding that the odds of cannabis use were higher for those who also consume alcohol, smoke and use e-cigarettes was in keeping with other research.
“The fact that adolescents are likely to engage in polysubstance use is significant and needs to be factored into any interventions targeting cannabis prevention among adolescents in Ireland,” said Dr O’Dowd.
The study also claimed there has been a cultural shift both nationally and internationally over the past decade towards legalising cannabis.
Dr O’Dowd said it had led to an attitude among many adolescents and adults that cannabis is a relatively harmless drug.
“This shift in perception regarding cannabis-related harm may impact Irish adolescents’ decision to use cannabis, as suggested by our findings,” she added.
The authors of the study said its findings had demonstrated the importance of parental attitudes to cannabis and claimed many factors including parental supervision and perception that parents are against cannabis use were “modifiable.”
They called for the public health community and policymakers to act to ensure greater awareness of cannabis harms among both teenagers and their parents.
“A tailored public health messaging campaign addressing the known harms and complications of cannabis use in young people, is urgently required,” they added.
Public News Service – Terri Dee, Anchor/Producer – Monday, January 6, 2025
One popular New Year’s resolution is to quit alcohol consumption.
Although easier said than done, one recovery center said there are modifications to try if previous attempts are not working. A good start is taking a hard look at what has worked and what has not.
Marissa Sauer, a licensed clinical addiction counselor at Avenues Recovery, a Fort Wayne recovery center, pointed out if there was a simple answer, everybody would use it. She added other influences are linked to alcohol and substance abuse.
“There’s genetics. Were my parents and my grandparents struggling with substances? Does someone have maybe adverse childhood experiences that have led to substances being a coping mechanism of some kind?” Sauer explained. “Maybe there are these mental health diagnoses.”
Sauer mentioned people, places, or things which could inhibit or enable someone to abuse drugs or alcohol, making it complicated to simply walk away. Medication, therapy or conversations with people who have beaten their addictions are all effective measures for recovery.
The US Surgeon General’s 2025 Advisory Report indicates alcohol consumption is the third leading preventable cause of cancer after tobacco and obesity and the public is taking notice.
There is a growing momentum of the “sober curious” movement, avoiding happy hours at bars, ordering a low or no-alcohol drinks known as mocktails, or completely abstaining from alcohol for 30 days for “dry January.” Sauer said longtime substance abusers fear change and she wants them to know there is hope.
“Whether you’re 21 or whether you’re 51, that ability to heal is there,” Sauer emphasized. “The best gift that you could give yourself for a healthy 2025 is to give your loved ones the absolute best version of yourself.”
An Indiana State Epidemiological report from 2021-2022 revealed almost 24% of residents aged 12 and older have participated in binge drinking, with the highest rate among young adults aged 18 to 25.
Source: https://www.publicnewsservice.org/2025-01-06/alcohol-and-drug-abuse-prevention/in-substance-recovery-center-supports-sober-existence/a94456-1
The Children’s Mercy Hospital psychiatrist more often hears from parents wondering if cannabis could help their child’s anxiety, autism or OCD.
“I tell them there are no studies,” said Batterson, the medical associate director of the hospital’s Division of Developmental and Behavioral Health. “A lot of hype, but no studies.”
And even if Children’s Mercy allowed its doctors to prescribe weed (it doesn’t), Batterson wouldn’t know what dose to recommend. He also couldn’t say which patient might experience a marijuana-induced psychotic episode or other serious reaction.
No one could.
Years of federal prohibition and the resulting limits on research mean the science about marijuana is skimpy at best. Public health experts say that should trigger caution in a world where legal marijuana is increasingly accessible and more widely consumed.
“There has been relatively little research on cannabis,” said Steven Teutsch, who chaired a year-long study for the National Academies of Sciences, Engineering and Medicine about the impact legal cannabis is having on public health. “Many of the benefits are often over-promoted and are iffy in many cases. And the harms are often not fully appreciated.”
Despite a well-known and largely accepted narrative that marijuana is safe and not addictive, the reality — especially when people consume greater and stronger amounts of the drug — is often different, health experts said.
Some 30% of cannabis users report having a physical dependency on the drug, according to the U.S. Centers for Disease Control and Prevention. Scientists believe the drug could hurt brain function, heart health and can lead to impaired driving. It also correlates with social anxiety, depression and schizophrenia.
The federal government, which Teutsch said has “ largely been missing in action in all of this,” needs to step in with campaigns to educate the public, with model legislation to help states regulate the drug and with research funding to study health effects — good and bad.
Marijuana is still illegal at the federal level, and classified by federal law as a Schedule I drug, defined as a highly addictive substance with no known medical use. Hearings on a proposal to reclassify it as a Schedule III drug will begin in January.
That change would remove barriers — and free more money — for research that could give doctors a better understanding of the health effects of all those gummies, pre-rolled joints and THC-spiked drinks at your neighborhood dispensary.
It also could pave the way for more drug development. To date, the U.S. Food and Drug Administration has only approved three drugs related to cannabis.
Some experts also contend that Congress needs to undo federal law adopted in 2018 that allowed hemp products containing THC (tetrahydrocannabinol), the primary psychoactive compound in cannabis, to be sold in gas stations and grocery stores, free from regulatory oversight.
Under the current system, every state with legal weed takes a different approach to the drug.
California became the first to legalize medical marijuana in 1996. And Colorado and Washington led the way in legalizing recreational pot in 2012.
In the years since, only a handful of states, including Kansas, have resisted passing some level of legalization. Missouri voters adopted a constitutional amendment allowing medical marijuana use in 2018, and one legalizing recreational weed in 2022.
The state has a responsibility, said Dr. Heidi Miller, chief medical officer for the Missouri Department of Health and Senior Services, to make sure people know the risks that come with marijuana.
“Cannabis has multiple potential therapeutic effects, but also potential adverse effects,” she said. “We need to inform the public of what we know and what we don’t know.”
Missouri has budgeted $2.5 million (less than 0.2% of what people in the state spend on weed in a year) for a public information campaign to get this message out.
Miller said the campaign, which is in early planning stages and not yet scheduled, should warn vulnerable populations — young people, pregnant or breastfeeding women and people with a personal or family history of mental illness — about the risks of getting high.
It should also alert people, she said, that the marijuana they may have smoked a few decades ago has little resemblance to the potent variety sold at dispensaries.
The stuff sold today may have four times more THC. And that doesn’t include concentrates, which can have THC levels reaching 90%.
“Clearly, the adverse effects are going to be heightened, the higher the potency,” Miller said. “We can’t assume that all cannabis is safe because it’s, quote, natural. We also want folks to understand that cannabis is potentially addictive.”
Since sales began in Missouri four years ago, the Division of Cannabis Regulation says more than $3 billion has been spent on cannabis products in the state. In fiscal year 2024, recreational sales, referred to as “adult use,” reached $1.16 billion, while medical weed sales totaled just under $166 million.
As in other states that have legalized cannabis, use of the drug is on the rise.
Dutchie, a technology company whose software powers the payment platforms and other backend systems in dispensaries, reported that on the Wednesday before Thanksgiving — known in the industry as “Green Wednesday” — average orders in Missouri dispensaries jumped 18% above a regular Wednesday to more than $84.
The number of people using the drug, which experts said will only continue to rise, is raising alarms.
A November 2023 report from the Substance Abuse and Mental Health Services Administration found that 61.9 million Americans — 22% of those 12 and older — reported using cannabis in the past year. More than 13 million 18 to 25 year olds — 38% — said they’d used the drug. The same was true for 11.5% of 12 to 17 year olds.
As people consume marijuana more frequently and in higher doses, anecdotal stories related to health problems are becoming more common. They include reports of cannabinoid hyperemesis syndrome, a gastrointestinal condition that leads to bouts of vomiting and intense pain, and instances of cannabis-induced psychosis, a mental illness that can lead to violence and suicide.
“They didn’t legalize old school hippy weed,” said Aubree Adams, a Colorado mother whose son became psychotic after using marijuana. “We’re dealing with a really hard drug.”
Every day, Adams said, the organization she founded to educate the public about the dangers of marijuana use, receives inquiries from a handful of families across the country dealing with issues related to marijuana use.
Her organization, Every Brain Matters, is pushing for potency caps on the marijuana being sold in the United States; an end to the sale of edibles, which often look like candy; and a ban on sugary-flavored vapes.
Adams also wants it to be illegal for marijuana companies to market products as medicine that have not been approved for medical use. States need to be out front telling the public the truth, she said.
“I don’t know why we have to sugar coat things and play politics,” she said. “Tell them the truth. Tell them the science.”
Her son is 24 now. He’s come in and out of sobriety since first getting into trouble “dabbing” highly concentrated marijuana when he was 15. She believes he would be fine if he hadn’t used the drug.
“My son fights for his mental well being on a daily basis,” she said.
Adams wants other parents to know the potential risks. And she wants adolescents and young adults — who she believes are a primary target of marijuana companies — to realize what they might be getting into. Doctors say that developing brains are more vulnerable to problems
“This is not a soft drug,” she said. “This is a hard drug that can change your brain chemistry.”
But getting meaningful regulatory change in an industry that lacks federal oversight is difficult.
Under the current system, every state has its own set of rules about everything from how cannabis products are packaged, tested and sold to what training the budtender at your local cannabis store needs to have. States decide who can buy cannabis, how much someone can buy during a certain period and how potent weed can be.
The states also oversee what’s in the marijuana, including setting maximum levels for contaminants like heavy metals and pesticides. Missouri’s Cannabis Division established rules based on the amendments voters adopted.
The state has licensed 10 private laboratories, which marijuana producers hire to test products for compliance with state rules. Cannabis regulators also are opening a “reference laboratory” by mid-2025 to verify those results.
Because the state legalized weed later than other states, it adopted standards that are among the most stringent in the country, said Anthony David, chief operations officer with Green Precision Analytics, a private marijuana testing lab in Kansas City. Before opening the lab with three partners, he grew marijuana in the Pacific Northwest.
“Cannabis that Missourians are smoking,” he said, “is safer than probably anywhere in the world.”
The National Academies of Sciences’ report on cannabis and public health, which was commissioned by the CDC and the National Institutes of Health, recommended several policy changes states could make to protect the public.
Those include things like limiting the potency of marijuana (Missouri has no such limit), and restricting retail hours at dispensaries. While Kansas City limits how late a dispensary can stay open, the state does not, and some weed shops in neighboring communities offer 24-hour-a-day drive-thrus. Other suggested policies from the report involve implementing strategies to protect kids. In short, they want cannabis products to be controlled much like alcohol and tobacco.
“Almost every state does something right, but there are a lot of things they don’t do,” Teutsch said. “We advise the states to look at what was done for tobacco and alcohol because there’s many years of experience there implementing policies that have a public health focus.”
David G. Evans, a New Jersey attorney representing people who claim they’ve been harmed by marijuana, also believes there is wisdom to be gained from what unfolded in the tobacco industry.
He contends that the legal system needs to step in where regulators have failed. Evans is suing marijuana companies for harming clients and marshalling lawyers across the country to do the same. He hopes the legal actions will bring public awareness about risks of marijuana and rein in the industry.
“The marijuana industry is low-hanging fruit,” Evans said. “They’ve been allowed to be reckless. They’ve not been controlled, not disciplined. And the state governments have played right along with them. Now there’s starting to be a reckoning.”
Source: https://www.ksmu.org/news/2024-12-28/with-weed-legal-missouri-is-now-looking-at-the-public-health-consequences
This story was originally published by The Beacon, a fellow member of the KC Media Collective.
New York Times DNYUZ December 26, 2024
The cartel operatives came to the homeless encampment carrying syringes filled with their latest fentanyl formula. The offer was simple, according to two men living at the camp in northwest Mexico: up to $30 for anyone willing to inject themselves with the concoction.
One of the men, Pedro López Camacho, said he volunteered repeatedly — at times the operatives were visiting every day. They watched the drug take effect, Mr. López Camacho said, snapping photos and filming his reaction. He survived, but he said he saw many others who did not.
“When it’s really strong, it knocks you out or kills you,” said Mr. López Camacho of the drugs he and others were given. “The people here died.”
This is how far Mexican cartels will go to dominate the fentanyl business.
Global efforts to crack down on the synthetic opioid have made it harder for these criminal groups to find the chemical compounds they need to produce the drug. The original source, China, has restricted exports of the necessary raw ingredients, pushing the cartels to come up with new and extremely risky ways to maintain fentanyl production and potency.
The experimentation, members of the cartels say, involves combining the drug with a wider range of additives — including animal sedatives and other dangerous anesthetics. To test their results, the criminals who make the fentanyl for the cartels, often called cooks, say they inject their experimental mixtures into human subjects as well as rabbits and chickens.
If the rabbits survive beyond 90 seconds, the drug is deemed too weak to be sold to Americans, according to six cooks and two U.S. Embassy officials who monitor cartel activity. The American officials said that when Mexican law enforcement units have raided fentanyl labs, they have at times found the premises riddled with dead animals used for testing.
“They experiment in the style of Dr. Death,” said Renato Sales, a former national security commissioner in Mexico. “It’s to see the potency of the substance. Like, ‘with this they die, with this they don’t, that’s how we calibrate.’”
To understand how criminal groups have adapted to the crackdown, The New York Times observed fentanyl being made in a lab as well as a safe house, and spent months interviewing several people directly involved in the drug’s production. They included nine cooks, three chemistry students, two high-level operatives and a recruiter working for the Sinaloa Cartel, which the U.S. government blames for fueling the synthetic opioid epidemic.
The people connected to the cartel spoke on the condition of anonymity for fear of retaliation.
One cook said he recently started mixing fentanyl with an anesthetic often used in oral surgery. Another said the best additive he had found was a sedative for dogs and cats.
Another cook demonstrated for Times reporters how to produce fentanyl in a cartel safe house in Sinaloa State, in northwest Mexico. He said that if the batch was too weak, he added xylazine, an animal tranquilizer known on the street as “Tranq” — a combination that American officials warn can be deadly. “You inject this into a hen, and if it takes between a minute and a minute and a half to die, that means it came out really good,” the cook said. “If it doesn’t die or takes too long to die, we’ll add xylazine.”
The cooks’ accounts align with data from the Mexican government showing a rise in the use of fentanyl mixed with xylazine and other substances, especially in cities near the U.S. border.
“The illicit market gets much more benefit from its substances by cutting them with different things such as xylazine,” said Alexiz Bojorge Estrada, deputy director of Mexico’s mental health and addiction commission.
“You enhance it and therefore need less product,” said Ms. Bojorge, referring to fentanyl, “and you get more profit.”
U.S. drug researchers have also noticed a rise in what one called “weirder and messier” fentanyl. Having tested hundreds of samples in the United States, they found an increase in the variety of chemical compounds in fentanyl on the streets.
“It’s just a wild west of experimentation,” said Caleb Banta-Green, a research professor at the University of Washington School of Medicine, who helped coordinate the testing of more than 580 samples of drugs sold as fentanyl in Washington State this year.
He called it “absolute chaos.”
The Experiments: The synthetic opioids that reach American streets often begin in cartel labs, where precision is not always a priority, cooks say. They mix up vats of chemicals in rudimentary cook sites, exposing themselves to toxic substances that make some cooks hallucinate, wretch, pass out and even die. The cartels are actively recruiting university chemistry students to work as cooks. One student employed by the cartel revealed that to test their formulas, the group brought in drug users living on the street and injected them with the synthetic opioid. No one has ever died, the student said, but there have been bad batches. “We’ve had people convulse, or start foaming at the mouth,” the student said.
Mistakes by cooks were met with severe punishment, she added: Armed men locked the offenders in rooms with rats and snakes and left them there for long stretches with no food or water.
The cooks and high-level operatives described the Sinaloa Cartel as a decentralized organization, a collection of so many disparate cells that no single leader or faction had complete control over the group’s fentanyl production.
Some cooks said they wanted to create a standardized product that wouldn’t kill users. Others said they didn’t see the lethality of their product as a problem — but as a marketing tactic.
In a U.S. federal indictment against the sons of the notorious drug lord Joaquín Loera Guzmán (known as El Chapo) who lead a powerful faction of the Sinaloa Cartel, prosecutors said the group sent fentanyl to the United States even after an addict died while testing it in Mexico.
Instead of scaring people off, cartel members, drug users and experts say that many American users rush to buy a particularly deadly batch because they know it will get them high.
“One dies, and 10 more addicts are born,” said one high-level operative for the cartel. “We don’t worry about them.”
The Boss: The boss knew something was wrong when the hens stopped keeling over. He said he’d been in the drug business since he was 12, when he started apprenticing at a heroin processing site.
Now a soft-spoken 22-year-old, the boss said he taught himself how to produce illicit drugs by studying the older, more experienced men he worked with. Eventually, he started his own business with a friend.
The boss said his business grew so fast that soon he was running three fentanyl labs. The drug has made him millions, he said.
Every time he goes to one of his labs, he said he brings four or five rabbits from the local pet store. If the fentanyl his people make is potent enough, he has to inject and kill only one to be sure it is fit for sale.
Two pet store employees in Sinaloa, who spoke on the condition of anonymity for fear of retaliation from cartel members, confirmed that the cheapest rabbits are known to be purchased for drug testing.
The boss’s other test subjects are hens from a nearby ranch. Many fentanyl cooks test their product on chickens, according to the two U.S. Embassy officials.
Until recently, the boss said every time he injected the hens with fentanyl they would either die, fall over or stumble around as if they were drunk. All the locals knew not to eat the chickens or the eggs from the ranch.
But recently, the animals weren’t having a strong reaction to the drug, even though his process hadn’t changed.
His employees were logging the same hours at the same modest lab in the mountains, starting at 5 a.m. and sleeping there for days on end. They were working with the same equipment — laboratory shakers, trays, large containers and a blender to mix up the final product.
The boss said he eventually concluded that the culprit was a “very diluted” supply of the chemical ingredients from China. The result was a bunk product. “It’s too weak,” he said.
To fix the problem, the boss first tried combining fentanyl with ketamine, a short-acting anesthetic, but said users didn’t like the bitter taste that came with smoking the mix. It worked much better to add procaine, he said, a local anesthetic often used to numb small areas during dental procedures. When asked whether he felt guilty about producing a drug that causes mass death, the boss said all he was doing was giving his customers what they wanted.
“If there weren’t all those people in the United States looking to get high, we wouldn’t sell anything,” he said. “It’s their fault, not ours. We just take advantage of the situation.”
The Cook
One cook we spoke with said he got into the fentanyl business a few years ago to pay off growing debts. At first, the former shop owner regularly got sick from the exposure to the fumes. He said the armed cartel members in charge had no patience for it.
“You may throw up at the beginning when you start, and you take a quick break and take some air,” said the cook, but soon enough “one of them will scream at you to get back to work.”
A boss once shot him just because he didn’t answer a question quickly enough, he said, pulling up his shirt to reveal a stomach scar.
He is constantly experimenting with ways to make fentanyl stronger, tweaking his formula and testing it on his lab assistants, many of whom have become addicted in the process, he said. If the product comes out strong, he passes it on to his supervisors to try.
The cook said he knows all the improvisation adds up to an unpredictable product. Each batch he makes is different, he said, meaning clients who buy the exact same fentanyl pills may get wildly different doses from week to week.
He’s never fully disclosed his job to his family, simply saying he’s off to work and then returning weeks later with a lot of cash. He believes the money and the fear evident in his expression deter any questions.
“There is no retirement here,” the cook said, adding that the cartel would likely kill him for trying to stop. “There is just work and death.”
Source: https://dnyuz.com/2024/12/26/how-mexican-cartels-test-fentanyl-on-vulnerable-people-and-animals/
__
—
www.drugwatch.org
drug-watch-international@googlegroups.com
Pharmacists can help address nicotine addiction by recommending FDA-approved smoking cessation methods and educating on the risks associated with electronic cigarette use.
Electronic cigarettes (E-cigarettes) have emerged as a popular alternative to traditional smoking. This method, known as vaping, involves inhaling an aerosol that contains nicotine, flavorings, and harmful chemicals including carcinogens, toxic substances, and metals. Nicotine is a highly addictive compound that activates the brain’s reward center by increasing dopamine levels, which creates sensations of pleasure and satisfaction. These euphoric feelings are often what leads to nicotine addiction.1
Although vaping is often perceived as a safer option, it actually carries significant health risks similar to those of traditional cigarettes. Pharmacists can play a vital role in educating patients on the dangers of vaping and providing guidance on safe and effective smoking cessation methods.
E-cigarettes trace back to the 1960s when British American Tobacco created a smoking device under the codename Ariel. At that time, researchers were already aware of nicotine’s addictive properties, but new evidence linking smoking to lung cancer prompted cigarette companies to try and explore alternative products with less risks. They aimed to create an inhalation device with filters to reduce carcinogens and tar. However, it was discovered that filtered cigarettes were not a healthier alternative because all components of cigarette smoke have proven to be harmful. Additionally, if the device only contained pure nicotine, it would warrant classification as a drug-delivery system, subjecting it to stricter regulations. The company wanted to avoid this in order to bypass the stringent safety evaluations and extensive clinical trials required by drug delivery systems, which would allow the company to reduce their manufacturing costs, speed up production, and take this device to the market quicker. They were able to produce a product with 24% nicotine, which is 6 times the concentration found in traditional cigarettes. Despite this innovation, Ariel was discontinued to protect the company’s profitable traditional cigarette market. This marked the first instance of companies exploring the manipulative potential of nicotine.2
E-cigarettes were officially authorized for sale by the FDA in 2007 with over 460 brands. The most popular brand is Juul, accounting for nearly 75% of the e-cigarettes on the market.3,4 In 2022, the FDA banned the sale of Juul products due to conflicting evidence regarding its associated risks, including the potential to cause strokes, respiratory failure, seizures, and cases of e-cigarette or vaping-use-associated lung injury (EVALI).4 EVALI is a condition in which the lungs become severely damaged and often results in admission to the intensive care unit (ICU) on mechanical ventilation.3,4
Additionally, there is also a lack of long-term safety data for these products.5 Although originally marketed as a healthier alternative to cigarettes, e-cigarettes have not demonstrated efficacy as a smoking cessation aid and rather, have led to a rise in the youth vaping epidemic.1
There has been a lack of data correlating successful smoking cessation rates among those who use e-cigarettes. There have been a few studies that suggest that vaping may aid in quitting tobacco but is not effective for quitting nicotine use altogether.6 One study found that those who utilized e-cigarettes in combination with nicotine replacement therapy (NRT) and counseling were 24.3% less likely to quit smoking compared to those who used only NRT and counseling. Additionally, those who used e-cigarettes were 15.1% more likely to become dual users utilizing both tobacco and vaping products. Those who are considered dual users are at an even higher risk for health complications including myocardial infarction and a 4-fold increase in developing lung cancer.6
In another survey of 800 people who utilized vaping as a smoking cessation agent, it was reported that only 9% successfully quit when asked 1 year later, compared to 19.8% who utilized NRT.1,7 These findings help highlight that vaping is not a reliable method for eliminating nicotine use entirely and can even lead to utilizing both traditional and electronic cigarette products.8
Vaping is now the most commonly used form of nicotine among adolescents. A study was conducted that showed high schoolers who had used e-cigarettes were 16.7% more likely to start smoking cigarettes within the next year.9 Nicotine’s impact on the developing brain can cause mood disorders, affect attention and learning, and amplify the desire for other mood-enhancing drugs such as cocaine or methamphetamine.1 In 2018, e-cigarette use among high school students increased by 78%, which led the FDA to enforce stricter regulations on the sale of nicotine products. Despite their efforts, vaping remains a leading challenge that teens face today as they have already fallen victim to nicotine addiction.4
The FDA currently lists 7 approved quit aids that are safe and effective for smoking cessation. These include several forms of NRT as well as pharmacologic therapy with bupropion and varenicline. Some of the agents, including the NRT gum, patch, and lozenge, are even available OTC. Pharmacists can play a vital role in smoking cessation, especially in patients who lack access to a primary care provider to obtain prescription medications. Therefore, it is crucial for pharmacists to stay up to date on the current smoking cessation guidelines, dosing recommendations, and counseling points for these agents.
The primary goal of pharmacist-driven smoking cessation should always be to support the patient’s desire to quit smoking. Pharmacists should guide patients toward the FDA-approved agents, either prescription medications through a provider, or OTC therapies in the pharmacy, rather than electronic cigarettes due to lack of supportive data and increased risk for adverse health events. The appropriate selection of FDA-approved agent should be individualized based on the patient’s specific factors, contraindications, and goals of therapy. Pharmacists should educate the patient extensively on the appropriate options for smoking cessation and should not recommend the use of e-cigarettes. However, if a patient decides to use e-cigarettes, pharmacists should still serve as a support system for the patient by being the primary educator and providing extensive counseling on the associated risks of vaping. Patients should be made aware of both the known and unknown adverse reactions associated with electronic cigarettes as well as highlighting that the goal of vaping should be to achieve complete smoking cessation.10
Vaping e-cigarettes has become a popular alternative to traditional cigarettes, with unknown efficacy and safety surrounding these products.10 Pharmacists should continue to stay up to date on new literature published on e-cigarettes and should follow the FDA’s suggestions on smoking cessation methods. Pharmacists are the most widely accessible health care professionals available to patients. Therefore, pharmacists have the power and knowledge to be the most influential providers available to advise patients on the correct paths to smoking cessation. By offering education and support, pharmacists can help patients live healthier lives and take steps towards reversing the youth smoking epidemic one education at a time.
Source: https://www.pharmacytimes.com/view/clearing-the-air-the-influence-of-vaping-on-smoking-cessation
What’s being said:
The details: It is possible the government’s efforts to disrupt drug trafficking and provide improved prevention, harm reduction and treatment services are beginning to achieve their desired effect.
But:
The larger context: The decrease is the largest in history, but the death toll remains high and disparities persist.
Source: White House takes credit for a big drop in fatal overdoses (Politico); Biden officials take credit for ‘largest drop’ in overdose deaths. Experts are more cautious (STAT); Future Threats (Politico)
Source: https://drugfree.org/drug-and-alcohol-news/policy-news-roundup-december-19-2024/
Gamblers Anonymous meetings are filling up with people hooked on trading and betting. Apps make it as easy as ordering takeout.
Wall Street Journal by Gunjan Banerji Dec. 20, 2024
A new type of addict is showing up at Gamblers Anonymous meetings across the country: investors hooked on the market’s riskiest trades.
At Gamblers Anonymous in the Murray Hill neighborhood of Manhattan, one man called options “the crack cocaine” of the stock market. Another said he faced hundreds of thousands of dollars in trading losses after borrowing from a loan shark to double down on stocks. And one young man brought his mom and girlfriend to celebrate one year since his last bet.
They were among a group of about 60 people, almost all men, who sat in rows of metal folding chairs in a crowded church basement that evening. Some shared their struggle with addiction—not on sports apps or at Las Vegas casinos—but using brokerage apps like Robinhood.
Many of the men, and scores of others around the country, discovered trading and betting during the pandemic boom that began in 2020. Some were drawn in by big wins in meme stocks and other viral stock sensations, leading them into even higher-octane wagers that offer the chance to put up a small amount of cash for a potentially mammoth return—or more often, a crushing loss.
Others bought and sold cryptocurrencies on apps that make trading as easy as ordering takeout on Uber Eats or toiletries on Amazon. In an age where sports betting has become an accepted pastime—accessible by the flick of the thumb on an iPhone app—they found the same rush betting on dogecoin, Tesla or Nvidia as wagering on Patrick Mahomes to carry the Kansas City Chiefs to the Super Bowl.
Doctors and counselors say they are seeing more cases of compulsive gambling in financial markets, or an uncontrollable urge to bet. They expect the problem to worsen. The stock market has climbed 23% this year and bitcoin recently topped $100,000 for the first time, tempting many people to pile into speculative trades. Wall Street keeps introducing newer and riskier ways to play the market through stock options or complex exchange-traded products that use borrowed money and compound the risk for investors.
Some who are desperate to stop trading are turning to self-help groups like Gamblers Anonymous. A GA pamphlet advises members to stay away from bets on stocks, commodities and options as well as raffle tickets and office sports pools. Sometimes members hand over retirement accounts to their spouses.
Modeled after Alcoholics Anonymous, GA dates back to 1957 and now has hundreds of chapters in every U.S. state. Attendees at local GA meetings from Ponca City, Okla., to Allentown, Pa., subscribe to a 12-step program. It begins with accepting that they are powerless over gambling and can include a financial review in a so-called pressure relief group meeting. New attendees are peppered with calls from others and latch onto veteran members who commit to helping them stay on track.
‘Hi, my name is Mitch’
More than 30 people interviewed by The Wall Street Journal, many of whom regularly attend GA meetings, said they’ve struggled with compulsive gambling in financial markets. At times, the trading led to mood swings, sleepless nights and even depression. Their trades—and spiraling losses—became a shameful secret that they kept from their partners or other loved ones.
I asked Gamblers Anonymous for permission to attend some meetings. Attendees introduced me to the groups at the start of the meetings, and I observed the discussions. Members introduced themselves by their first names, according to GA practices.
“Hi, my name is Mitch, and I’m a compulsive gambler,” one said at a GA meeting this month near Ozone Park, N.Y. “Hi Mitch,” the group responded in unison.
The suburban dad of three, slightly balding with a big smile, stood in front of more than a dozen members in a church basement. He is haunted by the rising price of bitcoin—and the riches that could have been his, he said. Up around 40% since Election Day, bitcoin prices are on a wild ride. What would have happened, he wondered out loud, if he had just left his bitcoin in a digital wallet and handed it over to his wife?
Then he reminded himself and the group that he was never able to just buy and hold. “I needed more and more,” Mitch told the group. “I’m a sick, compulsive gambler. That’s why I keep making these meetings. I don’t trust myself.”
One attendee told him to stop eyeing cryptocurrency prices. Another reminded him of the toll trading had taken on his family and asked: “What’s more important, crypto or your kids?”
The entrepreneur, based in Long Island, N.Y., said cryptocurrencies caught his eye when he was in his late 40s and had gone more than 20 years since placing his last bet. He had sworn off gambling after a penchant for bold bets had led him to Gamblers Anonymous meetings in his early 20s. He invested $100 in bitcoin and watched it soar. He poured thousands of dollars into ether and smaller, more speculative coins. Something kept him from sharing with his GA group that he was trading.
When his portfolio rose above $1 million, he thought to himself, “That’s four Lambos.” He flew to Florida to look at potential vacation homes for his family near Walt Disney World.
Within months, he found himself in a familiar cycle. The rush of adrenaline he got when he bought and sold tokens pushed him to trade more frequently—to the point where he was trading hundreds of times a day—and taking bigger risks. He would wake at 4 a.m. to monitor his portfolio.
He parked his car in the lot of a Long Island shopping plaza near his home to trade in isolation. His neck grew tense from hunching over the screen.
When crypto prices started tumbling, snowballing losses left him sullen. “Sometimes I would get a passing thought as I went to bed: I hope I don’t wake up in the morning,” he said. His portfolio had fallen around $1 million from its peak.
Desperate for a way out, he typed “crypto gambling treatment center” into Google. He confessed to his GA mentors that he had been gambling.
A spiking problem
Pennsylvania’s gambling hotline has fielded more calls tied to gambling in stocks and crypto since 2021 than it did in the prior six years combined. At a New York-based treatment center, Safe Foundation, clinical director Jessica Steinmetz estimates about 10% of patients are seeking help for addictions tied to trading. Before 2020, there were no such patients.
Lyndon Aguiar, a clinical director at Williamsville Wellness, a gambling treatment center in Hanover, Va., said counselors sit down with traders and delete dozens of stock, sports and financial news apps from their phones when they walk in the doors for its inpatient treatment program. The center has seen a 25% increase in gambling tied to markets since 2020, compared with the prior four years. Patients might install Gamban, an app that locks individuals out of gambling on their phones. The app started blocking Robinhood and Webull in July 2021.
A Robinhood spokesperson said it includes “robust safeguards to help customers make informed decisions” and that individuals deserve the freedom to become stewards of their own finances. A spokesperson for Webull said the platform offers educational tools to foster responsible investment decisions.
New patients often suffer from withdrawal symptoms including severe anxiety and depression when they first stop trading, he said. Some start fidgeting or repeatedly tapping their fingers against a table, itching to place a trade.
Abdullah Mahmood, administrative coordinator of a gambling program at the Maryhaven addiction treatment center in Columbus, Ohio, said he has seen several clients enter the treatment center’s doors this year for trading addictions. Options are particularly problematic, he said.
Activity in options is on track to smash another record this year. Trading in contracts expiring the same day, which are the riskiest, has soared to make up more than half of all trades in the market for S&P 500 index options this year, according to figures from SpotGamma. These trades are more electric than traditional stocks, with the potential to rocket higher or plunge to zero within minutes.
Similar to wagering on how many points Mavericks point guard Luka Dončić will score in the first quarter of an NBA game, traders are increasingly using options to speculate how stocks will fare during the trading session, rather than at the closing bell.
This year, “a client came down to my office, suicidal,” Mahmood said. “He had lost $14,000 in just five minutes in options trading on the app Robinhood.”
Doug Royer, 61, has been attending Mahmood’s group counseling sessions every Monday.
He initially entered the center’s doors for help with his drinking. Then, he saw signs for a gambling program while walking the halls of Maryhaven’s treatment center. Immediately, the six figures he lost trading came to mind.
After selling his house in 2022, he had poured thousands of dollars into investments like the Grayscale Bitcoin Trust, Lockheed Martin and Texas Pacific Land before amping up the risk with options trading. He traded in and out of companies such as Spirit Airlines and Estée Lauder, while borrowing on margin in an attempt to magnify his bets, brokerage statements show.
Eventually, he said he had almost no money left to trade with after losses in options and lotteries. He said he has been working part-time as a massage therapist near Columbus, Ohio. “It’s very easy to make a lot of money,” Royer said. “It’s also easy to lose everything really fast.”
Addiction counselors say gambling in financial markets often goes undetected and can be tough to track because individuals confuse their actions with investing. Unlike sports betting apps such as FanDuel and DraftKings, most brokerage apps don’t post warnings about gambling or offer hotlines to seek help. The proliferation of financial instruments, along with flashy brokerage apps that make them easy to trade, has also helped some gamblers convince themselves that they weren’t actually placing bets.
The National Council on Problem Gambling started including questions about investing in its annual survey in 2021, after its gambling hotline received an influx of calls during the meme-stock mania. The council’s executive director, Keith Whyte, said NCPG reached out to apps like Robinhood to suggest they adopt consumer protections ingrained in gambling apps. “In some cases, the consumer protections in the gambling industry exceed that in the financial markets,” Whyte said.
Like the anticipation of sex or delicious food, a financial gamble like an options trade can flood your brain with feel-good chemicals, said Brian Knutson, a professor of psychology and neuroscience at Stanford University. The bigger the financial payout or tastier the dish, the stronger the rush. That anticipation can keep a trader going back to place another bet, forming a reinforcing habit, added Knutson, who has studied risk-taking in financial markets for more than two decades.
“It’s not just the release, per se, of the dopamine, but the speed of the release that’s reinforcing,” Knutson said.
Chris Cachia, a 38-year-old power-plant technician in Ontario, Canada, got swept up with trading during the meme-stock mania in 2021. After turning around 7,000 Canadian dollars into roughly 50,000 trading stocks like GameStop and BlackBerry, he found short-dated stock options when he went hunting for fatter profits. He scored some early wins. Before long, the thousands he made evaporated and his account sank into a deep hole. Yet he said he couldn’t walk away—he was consumed by a fear of missing out on the riches that others boasted about online.
One week while his wife was traveling, he holed up in his home office for days trading. He grew desperate for a win and bet more money than he had in his brokerage account. It didn’t work out.
The subsequent loss left him so depressed that he skipped his brother’s bachelor party. “It was causing erratic changes in my behavior as I got deeper and deeper in,” Cachia said. “I was basically a full-out gambling addict.” He said he tried to quit countless times since his trading ramped up during the pandemic, deleting brokerage and social-media apps from his phone, only to quickly download them again. He wasn’t able to pull away until his wife threatened to leave him. “She gave me an ultimatum: You need to stop this, or I’m done,” Cachia said.
__
Source: More Men Are Addicted to the ‘Crack Cocaine’ of the Stock Market – WSJ

A decade ago, a stimulative drug that sold for just a few pounds, was banned in the UK. Known as khat, it’s a plant that’s chewed, giving similar effects to amphetamine.
Ten years on from the drugs reclassification, experts say it is still being sold in the UK, in places for ten times more than it cost in 2014.
But there is little data to help understand the true impact of the ban.
Dr Neil Carrier, who carried out postdoctoral research on the drug at the University of Oxford, said it has largely been “forgotten” by authorities and “in terms of understanding drug policy, the bans’ impact should really be researched”.
Mohammed, not his real name, 25, told the BBC that he tried khat in 2018, four years after the ban.
He said: “The thing is, there’s actually quite a lot of it readily available in the UK.
“You can get it in little silver sachet bags that are air-sealed and marketed as herbal facial products, but it’s literally just khat.”
He chewed the drug in a dried form, which has become more common during the past 10 years.
Dr Carrier, who currently works as a social anthropology professor at the University of Bristol, said fresh khat leaves were sold for “around £3 a bundle (250g)” during the 2000s and 2010s.
It was often chewed by Somali, Yemeni and Ethiopian men in group sessions at designated khat cafes, called mafrishes.
He helped produce a government-published literature review around khat’s social harms and legislation in 2011: “Very often as anthropologists, when we think about drugs, we don’t just focus on the drug itself but also how it gets caught up in the wider cultural meanings, wider relationships and power.
“We look at how it becomes a commodity and how the substance fits into society.”
He felt that the ban was a “missed opportunity” to investigate alternative methods of regulating recreational drugs.
“We could see how khat was associated with various issues that were very challenging with communities using khat in the UK.
“But at the time I felt the drug was blamed for these wider issues,” he said.
In the early 2000s Dr Carrier said he often heard people attribute khat to family and social integration problems.
“I would hear things like ’men are not being good fathers as they chewed khat’.
“And ‘people who are chewing khat might, as a consequence, not be looking for work’.
“But in reality, this is only half the picture.
“We often in society give drugs so much power and label them as the cause of problems when really the picture tends to be more blurred and complicated.”
Last year Border Force seized 2,760 hauls of class C drugs.
A Home Office spokesperson said: “Border Force and police work relentlessly to stop illegal drugs from coming into the country and keep them off our streets.
“We have seen a record level of seizures as we continue to use advanced technology, data and greater intelligence to ensure these drugs do not enter the country.”
The UK was one of the last EU countries to reclassify the khat in June 2014.
Prior to this date, more than 2,500 tonnes was annually imported, according to the Advisory Council of the Misuse of Drugs (ACMD).
That is the equivalent weight of around 208 double-decker buses worth of the stimulative drug.
Most of the shipments are thought to have been distributed and sold amongst east-African diaspora communities in Britain, such as Somalis and Ethiopians.
Dr Carrier said khat and cannabis, both plant-based drugs, have a similar policing system which could have contributed to a lack of data on how prevalent less drugs like khat may be.
“A lot of the drugs data gets conflated with data around cannabis and they tend to get pooled together.
“As far as I understand anyways,” he said.
UK Border Force tend to place khat into an “other class ” category, when reporting the drug.
Dr Carrier added: “What people suspected would happen at the time of the ban has happened.
“Khat is now being smuggled in, especially a dried khat, mostly coming in from Ethiopia, and it seems to have become quite popular.
“The people that do still want to consume, even though it’s been banned, can still consume it in a different form.”
Dried khat is less potent than the fresh plant and is said to provide a “less pleasant user experience” in terms of taste and texture.
Dr Carrier said that meant there is still a market for the drug: “Some people, if they can afford it, will still chew the fresh stuff.
“The fresh stuff is £30 to £40 a bundle.
“But there are people still willing to spend that kind of money on it.
“People are still accessing khat.”
Source: https://www.bbc.co.uk/news/articles/c4gpl62dn26o?utm_source=firefox-newtab-en-gb
Yijie Chen, PhD1; Xinyi Jiang, PhD1; R. Matthew Gladden, PhD1; Nisha Nataraj, PhD1; Gery P. Guy Jr., PhD1; Deborah Dowell, MD1
What is already known about this topic?
From 2020 to 2022, among overdose deaths with only illegally manufactured fentanyl (IMF) detected, those with evidence of smoking IMF increased by 78.9%, and those with evidence of injection decreased by 41.6%.
What is added by this report?
From July–December 2017 to January–June 2023, the percentage of persons injecting IMF sharply declined across all U.S. Census Bureau regions, with region-specific differences in magnitude; correspondingly, IMF snorting or sniffing increased in the Northeast, and IMF smoking increased in the Midwest, South, and West regions.
What are the implications for public health practice?
Whereas avoiding injection likely reduces infectious disease transmission, noninjection routes might still contribute to overdose. Provision of locally tailored messaging and linkage to medical treatment is important among persons using IMF through non-injection routes.
During 2019–2023, U.S. overdose deaths involving fentanyl have more than doubled, from an estimated 35,474 in 2019 to 72,219 in 2023 (1). From 2020 to 2022, overdose deaths with only illegally manufactured fentanyl (IMF) detected and evidence of smoking IMF increased by 78.9%; deaths with evidence of injection decreased by 41.6% (2). Smoking, however, could not be linked specifically to IMF use when deaths involved multiple drugs (e.g., methamphetamine co-used with IMF). To characterize IMF administration routes among all persons who use IMF, with or without other drugs, IMF administration routes were examined among adults assessed for substance use treatment who used IMF during the past 30 days.
The National Addictions Vigilance Intervention and Prevention Program’s Addiction Severity Index-Multimedia Version (ASI-MV) tool* includes a convenience sample of adults aged ≥18 years assessed for substance-use treatment. CDC analyzed treatment assessments conducted between July 1, 2017, and June 30, 2023, which were restricted to 14 states† with at least 100 assessments reporting past 30-day IMF use (16,636)§ and stratified by administration routes (swallowed, snorted or sniffed, smoked, and injected¶). The percentage of persons reporting each administration route was calculated for 6-month periods by U.S. Census Bureau region.** Significant (p-value <0.05) trends by administration route were identified using Joinpoint (Joinpoint version 5.1.0; National Cancer Institute) and Pearson correlations. This activity was reviewed by CDC, deemed not research, and was conducted consistent with applicable federal law and CDC policy.††
In the Midwest, South, and West U.S. Census Bureau regions, increases in smoking (from 7.8% during July–December 2017 to 38.2% during January–June 2023 [Midwest]; from 15.4% during January–June 2020 to 54.0% during January–June 2023 [South]; and from 45.7% during January–June 2018 to 85.7% during January–June 2023 [West]) were strongly negatively correlated with decreases in injection (Pearson correlation coefficient [r] = −0.96; p<0.001 [Midwest]; −0.98; p<0.001 [South]; and −0.74; p<0.01 [West]). Injection decreased from 75.2% during January–June 2020 to 41.2% during January–June 2023 in the Midwest U.S. Census Bureau region; from 54.2% during July–December 2020 to 30.3% during January–June 2023 in the South; and from 65.6% during July–December 2018 to 9.1% during January–June 2023 in the West, but timing of changes across each census region varied (Figure). In the Northeast, increases in snorting or sniffing (from 18.9% during July–December 2017 to 45.5% during January–June 2023) were strongly negatively correlated (r = −0.89; p<0.001) with a decrease in injection (from 83.8% during July–December 2017 to 63.4% during January–June 2023).
Consistent with other fatal overdose investigations (2), the percentage of persons injecting IMF sharply declined across all U.S. Census Bureau regions between 2017 and 2023, although the magnitudes of these declines were region-specific. Some persons who use IMF reportedly believe that smoking is safer than injecting IMF (3). Whereas avoiding injection likely reduces the risk for acquiring bloodborne viruses (e.g., HIV or HCV) and soft tissue infections (2,4), noninjection routes might contribute to overdose or other health problems (e.g., orofacial lesions associated with snorting) (5). Compared with injection, smoking IMF is associated with a higher frequency of use throughout the day and potentially higher daily dosages consumed (3). Substantial shifts to smoking IMF in the Midwest, South, and West, and sniffing or snorting IMF in the Northeast (i.e., Massachusetts) highlight the need to understand local trends in drug use and tailor local messaging, outreach, and linkage to medical care, including effective treatment for opioid use disorder in persons using IMF through noninjection routes.
Corresponding author: Yijie Chen, mns7@cdc.gov.
Source: https://www.cdc.gov/mmwr/volumes/73/wr/mm7350a4.htm?s_cid=mm7350a4_w
1Division of Overdose Prevention, National Center for Injury Prevention and Control, CDC.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflicts of interest were disclosed.
Millburn, NJ, Dec. 17, 2024 (GLOBE NEWSWIRE) — Thousands of residents from New Jersey and throughout the country, including many health care professionals, are now better informed and prepared to act in the fight against the nationwide opioid crisis thanks to the Knock Out Opioid Abuse Day Learning Series.
The Learning Series’ monthly webinars drew more than 10,000 attendees in 2024, including participants from fields including health care, education and law enforcement, as well as prevention, treatment and recovery professionals Organized by the Partnership for a Drug-Free New Jersey (PDFNJ) in collaboration with the Opioid Education Foundation of America (OEFA) and the Office of Alternative and Community Responses (OACR), the series covers a broad range of topics, from prevention and recovery to trauma, stigma and building resilience in those working on the front lines.
“The attendance represent thousands of people who are now better equipped to make a difference,” said Angelo Valente, Executive Director of PDFNJ.
Beyond educating the general public about the opioid epidemic, the series provided tools and strategies specific to health care workers and other professionals in related fields to help them make informed decisions in their work. Participants earned more than 6,000 continuing education credits, a testament to the program’s commitment to empowering professionals to drive real-world change in their communities.
The Learning Series provided credits for various professions including physicians, dentists, nurses, nurse practitioners, pharmacists, optometrists, social workers, certified health education specialists and EMTs.
In 2024, the webinars brought together experts from various prestigious institutions and organizations, including the New Jersey State Police, the Veterans Affairs Administration, and the Substance Abuse and Mental Health Services Administration (SAMHSA). These speakers, including Christopher M. Jones, Director of the Center for Substance Abuse Prevention at SAMHSA, shared practical solutions and cutting-edge research, ensuring participants left with insights that could be immediately applied in their communities.
“The Learning Series has grown steadily since it began in 2020, thanks to the incredible speakers and organizations that have shared their time and expertise,” Valente said. “Their contributions have made this series an invaluable resource for professionals in New Jersey and beyond, providing practical strategies and real-world insights to address the opioid crisis.”
The series also serves as part of the annual Knock Out Opioid Abuse Day initiative, held every October 6 to raise awareness about the risks of opioid misuse and educate residents and prescribers statewide. Its growth year over year underscores the need for evidence-based education and practical solutions to combat this epidemic.
The 2025 series will kick off at 11 a.m. on Thursday, January 30, 2025, with a webinar exploring the latest trends in the national opioid crisis. To learn more about Knock Out Opioid Abuse Day and for a schedule of webinars, please visit knockoutday.drugfreenj.org.
Source: https://www.morningstar.com/news/globe-newswire/9320021/2024-learning-series-drives-conversations-and-solutions-in-the-fight-against-opioid-misuse
<<<<<<<<<<<<<<<<<<<<<<<<<<>>>>>>>>>>>>>>>>>>>>>>
Best known for its statewide anti-drug advertising campaign, the Partnership for a Drug-Free New Jersey is a private not-for-profit coalition of professionals from the communications, corporate and government communities whose collective mission is to reduce demand for illicit drugs in New Jersey through media communication. To date, more than $200 million in broadcast time and print space has been donated to the Partnership’s New Jersey campaign, making it the largest public service advertising campaign in New Jersey’s history. Since its inception the Partnership has garnered 230 advertising and public relations awards from national, regional and statewide media organizations.
After declining significantly during the COVID-19 pandemic, substance use among adolescents has continued to hold steady at lowered levels for the fourth year in a row, according to the latest results from the Monitoring the Future Survey, which is funded by the National Institutes of Health (NIH). These recent data continue to document stable and declining trends in the use of most drugs among young people.
“This trend in the reduction of substance use among teenagers is unprecedented,” said Nora D. Volkow, M.D., director of NIH’s National Institute on Drug Abuse (NIDA). “We must continue to investigate factors that have contributed to this lowered risk of substance use to tailor interventions to support the continuation of this trend.”
Reported use for almost all measured substances decreased dramatically between 2020 and 2021, after the onset of the COVID-19 pandemic and related changes like school closures and social distancing. In 2022 and 2023, most reported substance use among adolescents held steady at these lowered levels, with similar trends and some decreases in use in 2024.
The Monitoring the Future survey is conducted by researchers at the University of Michigan, Ann Arbor, and funded by NIDA. The survey is given annually to students in eighth, 10th, and 12th grades who self-report their substance use behaviors over various time periods, such as past 30 days, past 12 months, and lifetime. The survey also documents students’ perceptions of harm, disapproval of use, and perceived availability of drugs. The survey results are released the same year the data are collected. From February through June 2024, the Monitoring the Future investigators collected 24,257 surveys from students enrolled across 272 public and private schools in the United States.
When breaking down the data by specific drugs, the survey found that adolescents most commonly reported use of alcohol, nicotine vaping, and cannabis in the 12 months prior to the survey, and levels generally declined from or held steady with the lowered use reported over the past few years. Compared to levels reported in 2023, data reported in 2024 show:
“Kids who were in eighth grade at the start of the pandemic will be graduating from high school this year, and this unique cohort has ushered in the lowest rates of substance use we’ve seen in decades,” said Richard A. Miech, Ph.D., team lead of the Monitoring the Future survey at the University of Michigan. “Even as the drugs, culture, and landscape continue to evolve in future years, the Monitoring the Future survey will continue to nimbly adapt to measure and report on these trends – just as it has done for the past 50 years.”
The results were gathered from a nationally representative sample, and the data were statistically weighted to provide national numbers. This year, 35% of students who took the survey identified as Hispanic. Of those who did not identify as Hispanic, 14% identified as Black or African American, 1% as American Indian or Alaska Native, 4% as Asian, 1% as Middle Eastern, 37% as white, and 7% as more than one of the preceding non-Hispanic categories. The survey also asks respondents to identify as male, female, other, or prefer not to answer. For the 2024 survey, 47% of students identified as male, 49% identified as female, 1% identified as other, and 3% selected the “prefer not to answer” option.
All participating students took the survey via the web – either on tablets or on a computer – with 99% of respondents taking the survey in-person in school in 2024. The 2024 Monitoring the Future data tables highlighting the survey results are available online from the University of Michigan.
The 2024 Monitoring the Future data tables highlighting the survey results are available online from the University of Michigan.
Source: https://nida.nih.gov/news-events/news-releases/2024/12/reported-use-of-most-drugs-among-adolescents-remained-low-in-2024
As the leading cause of a deregulation in the brain’s reward circuit, addictions are still widespread among the French population. This is largely due to the widespread use of legal psychoactive substances: tobacco and alcohol, which are the two leading causes of premature death in France. In 2020, nearly 25.5% of adults smoked every day (12 million people) and 10% drank at least one glass of alcohol a day (5 million people). So, what is the situation for substance addictions in France for the coming year?
First of all, to qualify as an addiction, a person must meet at least 2 of the 11 criteria set out in the Diagnostic and Statistical Manual of Mental Disorders (DSM‑5), including: craving, a compelling need to consume the substance or perform the activity; loss of control over the quantity and time devoted to consumption; increased tolerance to the product; a strong desire to reduce doses; continued use despite the damage; or the presence of a withdrawal syndrome when the addictive behaviour is abruptly stopped…
To date, only addictions to substances (tobacco, alcohol, cannabis, cocaine, opium and derivatives) or to video games and gambling are recognised as “addictions”. Social networking, sexual hyperactivity and sugar are not considered as such due to a lack of data and scientific evidence.
In France, the most widely used addictive substances are still tobacco, alcohol and cannabis. The first two are responsible for 75,000 and 41,000 deaths a year respectively. These are terrifying figures, known but ignored because of habit.
In an article published on 20 October 2024, Doctor Bernard Basset, chairman of the Addictions France association, and psychiatrist and addictologist Amine Benyamina, chairman of the Fédération Française d’Addictologie (FFA), proposed a series of measures combining public health and government debt, such as taxing drinks according to their alcohol content, or introducing a minimum price per drink based on the Scottish model. “In France, we have a real cultural problem with alcohol and very powerful lobbies,” says Amine Benyamina. “All public prevention policies are stifled or censored.” And yet, according to data collected by the Constances epidemiological cohort, which numbered almost 200,000 people in 2018, 19.8% of men and 8% of women in the working population are thought to have a harmful use of alcohol.
While the problem persists, it is changing. Starting with a major positive point made by Guillaume Airagnes, Director of the French Observatory of Drugs and Addictive Tendencies (OFDT) and Doctor of Psychiatry and Addictology: “The general consumption of substances such as tobacco and alcohol has been falling among young people since 2010.” However, there was a downside at the time of Covid, when several addictive activities were on the increase during confinement.
On the other hand, a clear increase in the use of psychostimulant drugs has been observed among adults since 2010, “although the levels of use in the general population remain incomparably lower than those for tobacco, alcohol or cannabis” points out Guillaume Airagnes.
These substances, like ecstasy, have benefited from their image becoming much more commonplace. This is also the case for cocaine, the availability of which has risen steadily over the last ten years, and which used to be the social marker of a wealthy economic category. In 2021, 26.5 tonnes of cocaine were seized, a 67% increase on 2018. “Cocaine benefits from the tenacious stereotype that it does not produce dependence. In reality, while the signs of physical withdrawal are almost non-existent, it is one of the most psychologically tyrannical substances, with extremely powerful cravings,” describes Amine Benyamina, who is also head of the psychiatry and addictology department at the Paul-Brousse hospital in Paris. This increase is set to continue. The 2020 lockdowns demonstrated the adaptability of the drug trade, with home delivery services, marketing, attractive packaging, the use of social networks and instant messaging, and even payments in cryptocurrency.
Another less well-known development is the misuse of certain opiate-based drugs, such as codeine or tramadol, which are intended for therapeutic purposes. These are morphine derivatives with a less powerful analgesic effect than morphine. “Paradoxically, this makes them more addictive,” explains Guillaume Airagnes. “As the psychoactive effects are less intense, this leads to greater compulsive consumption.” Misuse of these drugs has been documented for around ten years and remains under close surveillance, although it still only concerns a “very small proportion of users” the director of the OFDT points out.
In his department, Amine Benyamina also sees new types of drug misuse: “More marginal but just as problematic is the use of pregabalin or LYRICA. This is a product designed to treat neuropathic pain or post-traumatic stress syndromes.” This analgesic, which this time is not a morphine derivative, also has a strong addictive potential, encouraging patients to continue taking it beyond the prescription period.
One of the first problems facing carers is the lack of information about drug users themselves. In fact, most of the data on addiction in France comes from surveys carried out on the general population to be more representative. But not for much longer! In April 2024, the first national e‑cohort open only to drug users was launched: ComPaRe Pratiques Addictives. “We already have several thousand subscribers,” says Guillaume Airagnes, who is heading up the study. “The only condition to be eligible is to be a psychoactive substance user at the time of inclusion in the study. Of course, our aim is to follow up participants for at least 5 years, regardless of whether they continue to use substances.”
The responses and the long-term follow-up will enable Guillaume Airagnes and his teams to explore several avenues of research: the question of multiple drug use, which seems to be the rule rather than the exception; the relationship between drug use and economic, demographic or professional situation; the study of the very strong stigmatisation phenomenon among these users, etc. These data will also enable us to better target effective therapies that are adapted to each profile.
In its Guide pratique de psychothérapies les plus utilisées en addictologie of May 2022, the Fédération Française d’Addictologie lists and ranks the different therapies according to their clinical relevance. The behavioural and cognitive therapy (BCT) approach remains the most popular, with a method that can be adapted to addictions with and without substances and solid results confirmed by scientific studies.
But other avenues of treatment are being explored, such as the surprising use of LSD derivatives. “The initial results are surprising and encouraging,” says Professor Amine Benyamina with satisfaction. “Of course, it’s important to remember that these studies are very closely supervised” warns the professor, who is working with his team on the effect of psilocybin on alcohol addiction. “They should not be reproduced at home!”
SAM Drug Report’s Friday Fact report – 11:31 Friday 10th Jan 2025
A study that was published last week in Addictive Behaviors found that alcohol and tobacco are more likely to be used on days when marijuana is used.
The study found that individuals consumed an average of 0.45 more alcoholic drinks on days when marijuana was used, compared to days when marijuana was not used. Similarly, the study found that individuals smoked an average of 0.63 more cigarettes on days when marijuana was used. Both of these findings were statistically significant (p=0.01).
Seeking to explain these findings, the researchers posited that “the impact of cannabis use on the endocannabinoid system may reinforce the use of alcohol and tobacco through mechanisms related to psychological reward.” They added that “bidirectionality must be considered,” given that the use of one substance may influence the effect of an additional substance––it may enhance a high, for example.
The researchers noted that “the observed within-person positive associations between cannabis use and same-day alcohol consumption and cigarettes smoked are consistent with previous research that has shown a tendency for substance use behaviors to co-occur.”
Indeed, cross-tabs from the 2023 National Survey on Drug Use and Health found that those who used marijuana in the past 30 days were three times as likely to have smoked cigarettes in the past 30 days (30.8% vs. 10.4%) and 63% more likely to have used alcohol in the past 30 days (70.7% vs. 43.4%), compared to those who did not use marijuana in the past 30 days.
Source: SAM Drug Report’s Friday Fact report – 11:31 Friday 10th Jan 2025 – The Drug Report’s
Smart Approaches to Marijuana (SAM) is an alliance of organizations and individuals dedicated to a health-first approach to marijuana policy. We are professionals working in mental health and public health. We are bipartisan. We are medical doctors, lawmakers, treatment providers, preventionists, teachers, law enforcement officers and others who seek a middle road between incarceration and legalization. Our commonsense, third-way approach to marijuana policy is based on reputable science and sound principles of public health and safety.
People smoke the stuff perfectly openly, without fear, with the threatened £90 fine seemingly a remote possibility.
by Zoe Strimpel – The Telegraph London author – 14 December 2024 4:09pm GMT
Sir Elton John Credit: Ben Gibson
Zoe Strimpel writes: I was about 23 and was still finding my feet socially in London. I’d always really been a champagne girl at heart but cannabis smoking was common in some of the circles I spent time in. It seemed so tacky and boring, the province of the sorts of bores one met while “travelling”, so I usually said no.
But one night in a run-down flat somewhere in north London, I went along with everyone else. Not long afterwards my heart began to pound like never before and a wave of horrible panic crashed over me, like I was trapped in a physiological nightmare and might die.
This was combined with a much more familiar sense of self-recrimination: why had I got myself into this? It wasn’t tempting in the first place and it could never have been worth it. And now I was paying the price – and so was the friend, now more like a sister to me, who had to tend to me in my tearful panic.
Since then, the pressure to imbibe cannabis has only grown and spread, from tatty student settings to (upper)-middle class and middle-aged environs.
Those who prefer to avoid the smoke element can still mainline the active ingredient – THC – by choosing from a wide range of edibles, which are generally like jelly babies. These make you (me) feel just as dreadful as the smoke sort, though mercifully without the stink.
All of which is why I am in full agreement with Elton John who, as Time magazine’s “icon of the year”, has lambasted the legalisation of pot in North America as “one of the greatest mistakes of all time”.
Sir Elton, himself an addict until he got sober 34 years ago, pointed out that: “It leads to other drugs. And when you’re stoned – and I’ve been stoned – you don’t think normally.”
This is a statement of blinding obviousness, and yet in our strange society it sounds reactionary, refreshing, courageous. How is it that a drug known – outside of carefully managed medical settings where it can help with pain and sleep – to trigger psychosis and turn people into paranoiacs and dullards, and, when smoked, to cause damage to the lungs and body, came to be considered safe by North American lawmakers?
To be seen as so perfectly respectable, fine and dandy that states explicitly give their blessing to recreational use of it? And this in an America that doesn’t let people drink until they are 21 or even touch containers of alcohol till that age, or in public.
In the UK, it is not legal and classed as a class B drug. But that does not mean that ‘it is not ubiquitous’.
This is depressing. I’m all for the exploration and titration of psychoactive drugs to help people in desperate need of pain relief. I am interested in, though not yet convinced by, use of mushrooms (psilocybin) and ecstasy (MDMA) in treating depression.
But the general prevalence of cannabis is a much drearier, bigger, more worrying issue, connected to a general sense of inconsistency and disconnected logic among law-makers and enforcers on one hand, and a sense that all we want to do is bury ourselves in escapist hedonism that alters our minds and our worlds so as to reduce the stress associated with, for instance, responsibility, reality and work.
Labour has indicated that it does not wish to legalise cannabis. But it seems happy, as do the police, with the fact that nobody cares about its technical illegality. People smoke the stuff perfectly openly, without fear, with the threatened £90 fine seemingly a remote possibility. Children therefore have to inhale it in parks. It is a gateway drug for hard drugs and criminality, and forms a familiar backdrop for the insouciant menace of gangs.
But according 2023 figures from the ONS, cannabis was by far the most-commonly used recreational drug in the UK, with 7.4 per cent of adults aged 16 to 59 saying they had consumed it in the last year.
The counter-currents in state attitudes to recreational drugs are just weird. Why does the state look benignly on the smoking of this illegal substance, and fail to promote information about the dangers of inhaling it via smoke (and edibles), but noisily pursue the outlawing of cigarette smoking for those born after a certain date?
Fags are toxic and cancer-causing, and nobody should have to regularly breathe second-hand smoke. But so long as the harm of smoking (the tar in tobacco) is limited to the smoker, and those who voluntarily inhale their smoke, the wider mental effects are not disturbing.
Nicotine alone doesn’t tend to ‘alter personality beyond recognition’ or induce fits of paranoia, depression, criminality or addiction to other substances.
And let’s face it: a waft of cigarette smoke is quite pleasant. Cigarettes retain a kind of aesthetic glamour; their use is not at odds with beauty, comfort, decadence and good conversation. Pot-smokers, instead, give off a polluting stink that lowers the tone of whatever environment one is in, makes conversation a thousand times more inane, and seems to celebrate the urge to do less, or nothing, smugly. Cannabis is deadening, however it is consumed.
Even among those who work hard and have children, cannabis rules, becoming a fixation without which no relaxation is possible, whipped out as soon as the working day ends or the children are asleep. Perhaps what we need is to find other ways to relax, like reading a good book. Or, of course, to stop chasing relaxation and indolence at all costs, full stop.
SOURCE: https://www.telegraph.co.uk/news/2024/12/14/elton-john-is-right-cannabis-deadening-to-soul/
Alcohol is the leading driver of substance use-related fatalities in America: Each year, frequent or excessive drinking causes approximately 178,000 deaths.1 Excessive alcohol use is common in the United States among people who drink: In 2022, of the 137 million Americans who reported drinking in the last 30 days, 45% reported binge drinking (five or more drinks in a sitting for men; four for women).2 Such excessive drinking is associated with health problems such as injuries, alcohol poisoning, cardiovascular conditions, mental health problems, and certain cancers.3
In 2020, many people increased their drinking because of COVID-19-related stressors, including social isolation, which led to a 26% increase in alcohol-related deaths during the first year of the pandemic.4

Growth is driven by increases in both acute and chronic causes of death
Stacked bar graph shows yearly increases in alcohol-related deaths attributed to both chronic and acute causes from 2016-17 through 2020-21. Deaths related to chronic causes increased from approximately 89,000 to approximately 117,000 (a 32% increase), while acute deaths increased from approximately 49,000 to approximately 61,000 (a 24% increase).
Notes: Chronic causes of death include illness related to excessive alcohol use such as cancer, heart disease, and stroke, and diseases of the liver, gallbladder, and pancreas. Acute causes include alcohol-related poisonings, car crashes, and suicide.
Source: Marissa B. Esser et al., “Deaths From Excessive Alcohol Use—United States, 2016-2021,” Morbidity and Mortality Weekly Report 73, no. 8154-61, https://www.cdc.gov/mmwr/volumes/73/wr/mm7308a1.htm#T1_down
© 2024 The Pew Charitable Trusts
Nationwide, nearly 30 million people are estimated to have alcohol use disorder (AUD); it is the most common substance use disorder. AUD is a treatable, chronic health condition characterized by a person’s inability to reduce or quit drinking despite negative social, professional, or health effects.5 While no single cause is responsible for developing AUD, a mix of biological, psychological, and environmental factors can increase an individual’s risk, including a family history of the disorder.6
There are well-established guidelines for AUD screening and treatment, including questions that can be asked by a person’s health care team, medications approved by the U.S. Food and Drug Administration (FDA), behavioral therapies, and recovery supports, but these approaches often are not put into practice.7 When policies encourage the adoption of screening and evidence-based medicines for AUD, particularly in primary care, the burden of alcohol-related health problems can be reduced across the country.8
For adults of legal drinking age, U.S. dietary guidelines recommend that they choose not to drink or drink in moderation, defined as two drinks or fewer in a day for men, and one drink or fewer in a day for women.9 One drink is defined as 0.6 ounces of pure alcohol—the amount in a 12-ounce beer containing 5% alcohol, a 5-ounce glass of wine containing 12% alcohol, or 1.5 ounces of 80-proof liquor.10
Consumption patterns exceeding these recommended levels are considered:
Alcohol use disorder is defined by The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) as having symptoms of two or more diagnostic criteria within a 12-month period.13 The diagnostic criteria assess behaviors such as trying to stop drinking but being unable to, alcohol cravings, and the extent to which drinking interferes with an individual’s life.14 AUD can be mild (meeting two or three criteria), moderate (meeting four or five criteria), or severe (six or more criteria).15
Primary care providers are well positioned to recognize the signs of unsafe drinking in their patients. The U.S. Preventive Services Task Force recommends that these providers screen adults 18 years and older for alcohol misuse.16 One commonly used evidence-based approach, SBIRT—or screening, brief intervention, and referral to treatment—is a series of steps that help providers identify and address a patient’s problematic substance use.17
Using a screening questionnaire, a provider can determine whether a patient is at risk and, if so, can deliver periodic brief behavioral interventions in an office setting. Such interventions have been shown to reduce heavy alcohol use among adolescents, adults, and older adults.18 When a patient meets the criteria for AUD, providers can offer medication, connect them to specialty treatment, refer them to recovery supports such as Alcoholics Anonymous or other mutual-help groups, or all of the above, depending on a patient’s needs and preferences.19 When these interventions are used in primary care settings, they can reduce heavy alcohol use.20
While screening for AUD is common, few providers follow up when a patient reports problematic alcohol use. From 2015 to 2019, 70% of people with AUD were asked about their alcohol use in health care settings, but just 12% of them received information or advice about reducing their alcohol use.21 Only 5% were referred to treatment.22
Emergency departments (EDs) are another important setting for identifying AUD, and to maintain accreditation they are required to screen at least 80% of all patients for alcohol use.23 Alcohol is the most common cause of substance-related ED visits, meaning many people in these settings are engaged in excessive or risky alcohol consumption and could be linked to care.24
The use of SBIRT in the ED can also reduce alcohol use, especially for people without severe alcohol problems.25 Providers who use SBIRT can help patients reduce future ED visits and also some negative consequences associated with alcohol use, such as injuries.26
Commonly cited barriers to using SBIRT in these health care settings include competing priorities and insufficient treatment capacity in the community when patients need referrals. Conversely, SBIRT use increases with strong leadership and provider buy-in, collaboration across departments and treatment settings, and sufficient privacy to discuss substance use with patients.27
Jails and prisons should also screen for AUD, as well as other SUDs, to assess clinical needs and connect individuals with care. However, screening practices may not be evidence based. A review of the intake forms used to screen individuals in a sample of jails in 2018-19 found that some did not ask about SUD at all, and of those that did, they did not use validated tools accepted for use in health care and SUD treatment settings.28
Up to half of all people with AUD experience some withdrawal symptoms when attempting to stop drinking.29 For many, common symptoms such as anxiety, sweating, and insomnia are mild.30 For a small percentage, however, withdrawal can be fatal if not managed appropriately.31 These individuals can experience seizures or a condition called alcohol withdrawal delirium (also referred to as delirium tremens), which causes patients to be confused and experience heart problems and other symptoms; if untreated, it can be fatal.32 People with moderate withdrawal symptoms can also require medical management to address symptoms such as tremors in addition to anxiety, sweating, and insomnia.33
To determine whether a patient with AUD is at risk of severe withdrawal or would benefit from help managing symptoms, the American Society of Addiction Medicine recommends that providers evaluate patients with positive AUD screens for their level of withdrawal risk.34 Based on this evaluation, providers can offer or connect patients to the appropriate level of withdrawal management.35
At a minimum, high-quality withdrawal management includes clinical monitoring and medications to address symptoms.36 Providers may also offer behavioral therapies.37 Depending on the severity of a patient’s symptoms and the presence of co-occurring conditions such as severe cardiovascular or liver disease that require a higher level of care, withdrawal management can be provided on either an inpatient or an outpatient basis.38
According to the U.S. Department of Justice’s Bureau of Justice Assistance and the National Institute of Corrections, jails should also use evidence-based standards of care to address alcohol withdrawal. These standards include screening and assessing individuals who are at risk for withdrawal and, if the jail cannot provide appropriate care, transferring them to an ED or hospital.39
Withdrawal management on its own is not effective in treating AUD, and without additional services after discharge, most people will return to alcohol use.40 Because of this, providers should also connect people with follow-up care, such as residential or outpatient treatment, after withdrawal management to improve outcomes. Continued care helps patients sustain abstinence, reduces their risk of arrests and homelessness, and improves employment outcomes.41
Patients face multiple barriers to this follow-up care, however. For example, withdrawal management providers from the Veterans Health Administration cited long wait times for follow-up care, inadequate housing, and lack of integration between withdrawal management and outpatient services as reasons patients couldn’t access services.42 Patients have also cited barriers such as failure of the withdrawal management provider to arrange continued care, lengths of stay that were too short to allow for recovery to begin, insufficient residential treatment capacity for continued care, and inadequate housing.43
Promising practices for improving care continuity include: providing peer recovery coaches—people with lived expertise of substance use disorder who can help patients navigate treatment and recovery; psychosocial services that increase the motivation to continue treatment; initiating medication treatment before discharge; reminder phone calls; and “warm handoffs,” in which patients are physically accompanied from withdrawal management to the next level of care.44
In 2023, 29 million people in the U.S. met the criteria for AUD, but less than 1 in 10 received any form of treatment.45 Formal treatment may not be necessary for people with milder AUD and strong support systems.46 But people who do seek out care can face a range of barriers, including stigma, lack of knowledge about what treatment looks like and where to get it, cost, lack of access, long wait times, and care that doesn’t meet their cultural needs.47
For those who need it, AUD treatment can include a combination of behavioral, pharmacological, and social supports designed to help patients reach their recovery goals, which can range from abstaining from alcohol to reducing consumption.48
While for many the goal of treatment is to stop using alcohol entirely, supporting non-abstinence treatment goals is also important, because reduced alcohol consumption is associated with important health benefits such as lower blood pressure, improved liver functioning, and better mental health.49
Services for treating AUD—including medication and behavioral therapy—can be offered across the continuum of care, from primary care to intensive inpatient treatment, depending on a patient’s individual needs.50
Medications for AUD help patients reduce or cease alcohol consumption based on their individual treatment goals and can help improve health outcomes.51 Medications can be particularly helpful for people experiencing cravings or a return to drinking, or people for whom behavioral therapy alone has not been successful.52 But medications are not often used: Of the 30 million people with AUD in 2022, approximately 2% (or 634,000 people) were treated with medication.53
The FDA has approved three medications to treat AUD:
Additionally, some medications used “off-label” (meaning they were approved for treating other conditions) have also effectively addressed AUD. A systematic review found that topiramate, a medication approved for treating epilepsy and migraines, had the strongest evidence among off-label drugs for reducing both any drinking and heavy drinking days.68 Like naltrexone, it can reduce the incidence of alcohol-related liver disease.69
Despite the benefits that medications provide, they remain an underutilized tool for a variety of reasons—such as lack of knowledge among patients and providers, stigma against the use of medication, and failure of pharmacies to stock the drugs.70
Behavioral therapies can also help individuals manage AUD, and they support medication adherence:
All of these approaches can help address AUD, and no one treatment has proved more effective than another in treating this complicated condition.76 Combining behavioral therapies with other approaches such as medication and recovery supports, as described below, can improve their efficacy.77
Peer support specialists and mutual-help groups can also help people achieve their personal recovery goals:
People with AUD can use recovery supports on their own, in combination with behavioral treatment or medication, or as a method to maintain recovery when leaving residential treatment or withdrawal management.82
While the U.S. records more than 178,000 alcohol-related deaths each year, some populations have a higher risk of alcohol-related deaths, and others face greater barriers to treatment.83
Despite seeking treatment at higher rates than other racial/ethnic groups, American Indian and Alaska Native people have the highest rate of alcohol-related deaths.84
Alcohol‑related deaths per 100,000 people
A clustered column chart displays the rate of alcohol-related deaths per 100,000 people by racial and ethnic group for four years: 2012, 2016, 2019, and 2022. While the chart shows increasing rates for all included racial and ethnic groups (American Indian/Alaska Native, White, Hispanic, Black, and Asian or Pacific Islander), the mortality rates are highest each year for American Indian/Alaska Natives.
© 2024 The Pew Charitable Trusts View image
Risk factors that impact these communities and can contribute to these deaths include historical and ongoing trauma from colonization, the challenges of navigating both native and mainstream American cultural contexts, poverty resulting from forced relocation, and higher rates of mental health conditions than in the general population.85 Substances, including alcohol, are sometimes used to cope with these challenges.86
However, American Indian/Alaska Native communities also have rich protective factors such as their cultures, languages, traditions, and connections to elders, which can help reduce negative outcomes associated with alcohol use, especially when treatment services incorporate and build on these strengths.87
For example, interviews with American Indian/Alaska Native patients with AUD in the Pacific Northwest revealed that many participants preferred Native-led treatment environments that incorporated traditional healing practices and recommended the expansion of such services.88
To improve alcohol-related outcomes for American Indians and Alaska Natives, policymakers and health care providers must develop a greater understanding of the barriers and strengths of these diverse communities and support the development of culturally and linguistically appropriate services. The federal Department of Health and Human Services Office of Minority Health defines such an approach as “services that are respectful of and responsive to the health beliefs, practices, and needs of diverse patients.”89
Rural communities are another group disproportionately affected by AUD. People living in rural areas have higher alcohol-related mortality rates than urban residents but are often less likely to receive care.90 They face treatment challenges including limited options for care; concerns about privacy while navigating treatment in small, close knit communities; and transportation barriers.91
2012‑22 change in alcohol‑induced death rate per 100,000 by urban and rural areas
A graph with four bars shows the increase in alcohol-related deaths per 100,000 people in urban and rural areas from 2012 to 2022. In urban areas, the rate increased from 8.6 to 14.9 per 100,000 people, a 73% increase. In rural areas, the rate increased from 10.1 to 19.6 per 100,000 people, a 94% increase.
Telemedicine can help mitigate these barriers to care.92 Cognitive behavioral therapy and medications for AUD can be delivered effectively in virtual settings.93 People with AUD can also benefit from virtual mutual-help meetings, though some find greater value in face-to-face gatherings.94
Despite the value of virtual care delivery, people living in rural areas also often have limited access to broadband internet, which can make these interventions challenging to use.95 Because of this, better access to in-person care is also needed.
To improve screening and treatment for patients with AUD, policymakers, payers, and providers should consider strategies to:
AUD is a common and treatable health condition that often goes unrecognized or unaddressed. Policymakers can improve the health of their communities by supporting providers in increasing the use of evidence-based treatment approaches.98
If you are concerned about your alcohol consumption, you can use the Check Your Drinking tool created by the Centers for Disease Control and Prevention to assess your drinking levels and make a plan to reduce your use.
Source: https://www.pewtrusts.org/en/research-and-analysis/fact-sheets/2024/12/americas-most-common-drug-problem-unhealthy-alcohol-use
From 2018 to 2022, the National Highway Traffic Safety Administration (NHTSA) recorded more than 4,700 deaths in drunk driving traffic crashes during the month of December. In addition, a study by NHTSA found more than 54% of injured drivers had some amount of alcohol or drugs in their system at the time of the incident.
Although this month focuses primarily on reducing impaired driving on the road, it’s also crucial to extend this conversation to safety in the workplace and how drunk and drug-impaired driving can impact the construction industry.
What can your organization do to prevent drunk and drug-impaired driving incidents?
NAHB has several Video Toolbox Talks available in English and Spanish regarding drunk and drug-impaired driving. Please be sure to check out our content and help spread awareness as we approach the holidays:
In addition, several government establishments are promoting materials during this time of year. Check out their available resources:
If you know of anybody that needs immediate help, please reach out to the 988 Suicide and Crisis Lifeline or SAMHSA’s National Helpline, 1-800-662-HELP (4357).
Source: https://www.nahb.org/blog/2024/12/promote-safe-driving-resources
Teen alcohol use has steadily decreased from 2000 to 2024 — falling from 73% to 42% in 12th grade, 65% to 26% in 10th grade and 43% to 13% in 8th grade — according to data from Monitoring the Future (MTF), an annual federally funded study.
Every year, the University of Michigan’s Institute for Social Research uses grant money from the National Institute on Drug Abuse to conduct the MTF main study, which surveys more than 25,000 8th, 10th and 12th graders to monitor behaviors, attitudes and values of adolescents.
Meanwhile, the MTF’s panel study does follow-up surveys with roughly 20,000 adults ages 19 to 65 to continue to track trends over time.
Binge drinking, which researchers defined as “consuming five or more drinks in a row at least once during the past two weeks,” among teens also declined in 2024 for all three grades compared to 2023 and the past two-and-half decades.
Since 2000, binge drinking has fallen from 30% to 9% in 12th grade, from 24% to 5% in 10th grade and from 12% to 2% in 8th grade.
Teen cigarette use in 2024 was the lowest ever recorded since the survey started tracking 12th graders in 1975 and 10th and 8th graders in 1991.
“The intense public debate in the late 1990s over cigarette policies likely played an important role in bringing about the very substantial downturn in adolescent smoking that followed,” researchers said, adding that “an important milestone occurred in 2009 with passage of the Family Smoking Prevention and Tobacco Control Act, which gave the U.S. Food and Drug Administration the authority to regulate the manufacturing, marketing, and sale of tobacco products.”
Researchers emphasized that “over time this dramatic decline in regular smoking should produce substantial improvements in the health and longevity of the population.”
Teen marijuana use (non-medical) in 2024 also declined for all three grades, with the percentage of students using marijuana in the last 12 months at 26% in 12th grade, 16% in 10th grade and 7% in 8th grade.
“Levels of annual marijuana use today are considerably lower than the historic highs observed in the late 1970s, when more than half of 12th graders had used marijuana in the past 12 months,” researchers reported.
OPENING STATEMENT BY AUTHOR: Dec 31, 2024
Drug Free Australia has launched a new Substack where we start out with the foundational failure of Australia’s 1985 Harm Minimisation experiment which has literally seen thousands of families (5,400 between 2000 and 2007 alone) needlessly grieving for a lost loved one – all directly as a result of our adoption of Harm Reduction measures. If you think this is fanciful, you need to look at the cold, hard evidence.
If you live in another country, this is precisely a drug policy approach you need to fight to avoid and you may need to use this data to do it.
Gary Christian, President, Drug Free Australia. Phone: 0422 163 141
Meant to reduce drug-related deaths and harm, Australia’s mortality quadrupled during the first 14 years from around 250 deaths in 1984 to 1,116 in 1999.
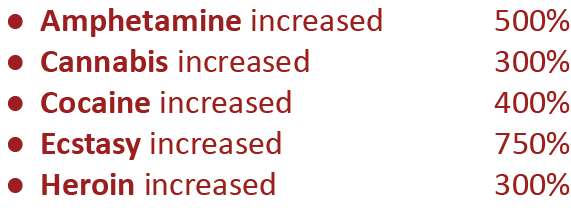
Looking at United Nations’ Drug Report figures for all countries worldwide, by 1998 Australia had the highest drug use amongst OECD countries, almost double that of the third, fourth and fifth highest countries. Only New Zealand, in second place, came close, having also adopted Harm Reduction programs in 1987
In 1998, the Federal Government, responding to community alarm at the unacceptable mortality, introduced a new approach called Tough on Drugs. Quadrupling the drugs budget to focus on prevention messaging, heavily expanded rehab and better policing of borders saw use of any illicit drug decrease by 39% and overdose deaths plummet by 67% by 2001, which is where mortality remained for 7 years. Throughout this period the Government chose not to close any Harm Reduction programs, which in light of this analysis, were simply running interference as an impediment to even better outcomes.
Nevertheless, this drug policy approach over a nine year period acted as a control by which the other two periods of Harm Reduction ascendency can be judged.
With a new Federal Government scrapping Tough on Drugs in 2007, prevention and rehab took a back seat, although heroin supply at the borders remained suppressed. And what happened was a virtual repeat of the first Harm Reduction era, demonstrating the same harm-multiplying dynamic. Yet with this official government graph below (with our added commentary overlaid) there is more to see than with the previous data.
In the decade following 2007 opiate deaths increased 260%, while other illicits drugs contributing to overdose deaths each increased 210%-590%. The reinstatement of a Harm Reduction priority was clearly a tide that lifted all boats.
We therefore find it conclusive that Harm Reduction has very demonstrably, substantially and consistently multiplied drug-related deaths and harm in this country.
Harm Reduction proponents will invariably claim that there is some hidden confounder that invalidates any conclusion, but the lockstep rise and fall of all drug types in concert with the differing drug policy eras rules out any major change in supply for any illicit (barring the 2000 heroin drought), just as it does with any possibility of a change in definition of a drug-related death. There are no viable confounders.
What is clear is that drug prevention and rehabilitation, as the first demand reduction pillar of Australia’s ‘Harm Minimisation’ approach, along with supply reduction at our borders, are both undermined by any ‘safe use of illicit drugs’ programming which is an explicit and implicit message of any harm reduction intervention.
Australia has given the world the gift of a viable ‘control’ drug policy period which ably shows the devastation caused by Harm Reduction.
It is time for the world to stand up and take notice. Hundreds of thousands of lives will be saved each year when all countries, including Australia, follow the lead of Australia’s Tough on Drugs policy.
___________________________________
** Harm Reduction, by definition, has no vested interest in drug prevention.
Source: https://open.substack.com/pub/drugfreeaustralia/p/how-harm-reduction-devastated-australia?r=1hnlai&utm_campaign=post&utm_medium=web
A study of nearly 10,000 adolescents funded by the National Institutes of Health (NIH) has identified distinct differences in the brain structures of those who used substances before age 15 compared to those who did not. Many of these structural brain differences appeared to exist in childhood before any substance use, suggesting they may play a role in the risk of substance use initiation later in life, in tandem with genetic, environmental, and other neurological factors.
This adds to some emerging evidence that an individual’s brain structure, alongside their unique genetics, environmental exposures, and interactions among these factors, may impact their level of risk and resilience for substance use and addiction. Understanding the complex interplay between the factors that contribute and that protect against drug use is crucial for informing effective prevention interventions and providing support for those who may be most vulnerable.”
Nora Volkow M.D., Director of NIDA
Among the 3,460 adolescents who initiated substances before age 15, most (90.2%) reported trying alcohol, with considerable overlap with nicotine and/or cannabis use; 61.5% and 52.4% of kids initiating nicotine and cannabis, respectively, also reported initiating alcohol. Substance initiation was associated with a variety of brain-wide (global) as well as more regional structural differences primarily involving the cortex, some of which were substance-specific. While these data could someday help inform clinical prevention strategies, the researchers emphasize that brain structure alone cannot predict substance use during adolescence, and that these data should not be used as a diagnostic tool.
The study, published in JAMA Network Open, used data from the Adolescent Brain Cognitive Development Study, (ABCD Study), the largest longitudinal study of brain development and health in children and adolescents in the United States, which is supported by the NIH’s National Institute on Drug Abuse (NIDA) and nine other institutes, centers, and offices.
Using data from the ABCD Study, researchers from Washington University in St. Louis assessed MRI scans taken of 9,804 children across the U.S. when they were ages 9 to 11 – at “baseline” – and followed the participants over three years to determine whether certain aspects of brain structure captured in the baseline MRIs were associated with early substance initiation. They monitored for alcohol, nicotine, and/or cannabis use, the most common substances used in early adolescence, as well as use of other illicit substances. The researchers compared MRIs of 3,460 participants who reported substance initiation before age 15 from 2016 to 2021 to those who did not (6,344).
They assessed both global and regional differences in brain structure, looking at measures like volume, thickness, depth of brain folds, and surface area, primarily in the brain cortex. The cortex is the outermost layer of the brain, tightly packed with neurons and responsible for many higher-level processes, including learning, sensation, memory, language, emotion, and decision-making. Specific characteristics and differences in these structures – measured by thickness, surface area, and volume – have been linked to variability in cognitive abilities and neurological conditions.
The researchers identified five brain structural differences at the global level between those who reported substance initiation before the age of 15 and those who did not. These included greater total brain volume and greater subcortical volume in those who indicated substance initiation. An additional 39 brain structure differences were found at the regional level, with approximately 56% of the regional variation involving cortical thickness. Some brain structural differences also appeared unique to the type of substance used.
While some of the brain regions where differences were identified have been linked to sensation-seeking and impulsivity, the researchers note that more work is needed to delineate how these structural differences may translate to differences in brain function or behaviors. They also emphasize that the interplay between genetics, environment, brain structure, the prenatal environment, and behavior influence affect behaviors.
Another recent analysis of data from the ABCD study conducted by the University of Michigan demonstrates this interplay, showing that patterns of functional brain connectivity in early adolescence could predict substance use initiation in youth, and that these trajectories were likely influenced by exposure to pollution.
Future studies will be crucial to determine how initial brain structure differences may change as children age and with continued substance use or development of substance use disorder.
“Through the ABCD study, we have a robust and large database of longitudinal data to go beyond previous neuroimaging research to understand the bidirectional relationship between brain structure and substance use,” said Alex Miller, Ph.D., the study’s corresponding author and an assistant professor of psychiatry at Indiana University. “The hope is that these types of studies, in conjunction with other data on environmental exposures and genetic risk, could help change how we think about the development of substance use disorders and inform more accurate models of addiction moving forward.”
Miller, A. P., et al. (2024). Neuroanatomical Variability and Substance Use Initiation in Late Childhood and Early Adolescence. JAMA Network Open. doi.org/10.1001/jamanetworkopen.2024.52027.
Source: https://www.news-medical.net/news/20241230/Structural-brain-differences-in-adolescents-may-play-a-role-in-early-initiation-of-substance-use.aspx
Published: December 31, 2024
DOI: 10.7759/cureus.76659
This is a large article. To access the full document:
There is undoubtedly an alarmingly rising trend of substance use among older adults. This has necessitated a paradigm shift in healthcare and propelled strategies aimed at effective prevention and screening. Age-related physiological changes, such as diminished metabolism and increased substance sensitivity, make older adults particularly vulnerable to adverse effects of substances. This not only has adverse psychological consequences but also physical consequences like complicating chronic illnesses and harmful interactions with medications, which lead to increased hospitalization.
Standard screening tools can identify substance use disorders (SUDs) in older adults. Tools like the Cut-down, Annoyed, Guilty, and Eye-opener (CAGE) questionnaire and Michigan Alcohol Screening Test-Geriatric (MAST-G) are tailored to detect alcoholism, while the Alcohol, Smoking, and Substance Involvement Screening Test (ASSIST) and Alcohol Use Disorders Identification Test (AUDIT) assess abuse of illicit and prescription drugs. Since older adults are more socially integrated, screening should be done using non-stigmatizing and non-judgmental language.
Prevention strategies include educational programs, safe prescribing practices, and prescription drug monitoring. Detection of substance abuse should be followed by brief interventions and specialized referrals. In conclusion, heightened awareness, improved screening, and preventive measures can mitigate substance abuse risks in this demographic. Prioritizing future research on non-addictive pain medications and the long-term effects of substances like marijuana seems justified.
SCOPE was formed in 2019 to help prevent opioid addiction, conducting cutting-edge research and education according to the announcement.
“The breakthroughs emerging from SCOPE’s work are paving the way for a future in which fewer families suffer the heart-wrenching loss of a loved one to an opioid overdose,” said Yost.
In addition to the announcement, Yost also shared a five-year report of SCOPE’s impact.
The SCOPE team includes Beth Delaney, Caroline Freiermuth, Tessa Miracle, Rene Saran, Jon E. Sprague, Donnie Sullivan, Julie Teater and Arthur B. Yeh.
The report includes four major sections titled “raising public awareness”, “educating future health-care professionals”, “emphasizing proper drug storage, disposal” and “prioritizing pharmacogenomics”.
Raising Public Awareness
The first section of the report outlines background information on the opioid issue the SCOPE was founded on. It also states that an underlying issue were illicitly manufactured fentanyls (IMFs) that are often added to other drugs.
The report goes on to state that work conducted by the Chemistry Unit in the Ohio Bureau of Criminal Investigation’s Laboratory found noteworthy comparisons of polydrug samples that included IMFs.
The most present IMFs in the polydrug samples during this study were fentanyl and para-fluorofentanyl.
In 2013, 2.2% of polydrug samples containing heroin and cocaine also contained IMFs. However, in 2022, more than 89% of polydrug samples contained IMFs. This is described as a 335-fold increase according to the report.
Also included in this section of the report was findings the committee reported when they conducted a longitudinal study of opioid overdose data from the Ohio Department of Health death records going back to 2007.
The findings included the fact that the death rate from opioid use per 100,000 reached 14.29 in the second quarter of 2020, the highest statistic to date in Ohio.
Educating Future Health-Care Professionals
In December 2019, SCOPE surveyed students enrolled in health-care professional programs at 49 of Ohio’s universities to see how many of these students were learning about “Opioid Use Disorder” (OUD).
The survey reportedly covered four main categories:
Results of the survey showed a need for a standardized curriculum discussing OUD.
SCOPE partnered with Assistant Professor Dr. Kelsey Schmuhl of Ohio State University’s College of Pharmacy to develop the “Interprofessional Program on Opioid Use Disorder”.
The more than 2,000 students that completed the course were suggested to understand more about OUD and the factors that contribute to it.
Emphasizing Proper Drug Storage, Disposal
A large danger that SCOPE wanted to address was the potential danger of having unsecured opioids available at home from left over prescriptions.
A study conducted by the Wisconsin Poison Control in which calls were fielded between 2002 and 2016 relating to unintended opioid exposure revealed that 61% of cases involved children aged zero to 5-years-old, and 29% involved teens between 13 and 19 years.
SCOPE partnered with the U.S. Drug Enforcement Administration to create the “Attorney General Drug Dropoff Days” which combine with the DEA’s Drug Take-back Days.
The report reflects on a map depicting a snapshot from the second quarter of 2020, showing that Ohio counties such as Scioto, Fayette and Franklin had the largest amounts of opioid overdose deaths.
Mahoning County and Trumbull County are also listed on this graphic.
To date, these events have been held in 11 counties throughout Ohio and have yielded over 2,600 pounds of unwanted and unsecured prescription medications.
Source: https://www.wfmj.com/story/52096722/scope-looks-back-on-the-progress-developments-of-its-past-five-years
In 2022 the White House Office of National Drug Control Strategy (ONDCP) published its first National Drug Control Strategy, which outlined seven goals to be achieved by 2025. On December 30, 2024, the ONDCP released the National Drug Control Strategy Performance Review System (PRS) Report—essentially a progress update on the Biden administration response to the overdose crisis between 2020 and 2022.
Though the ONDCP published an updated Strategy in May 2024, the new PRS report is intended to span data through 2022, corresponding to the original version. It has a tendency to veer into data from more recent years, however, which reflect a turnaround in overdose rates and as such look a lot better than the years the report is meant to cover.
The seven goals outlined in the original Strategy contain 25 objectives, most of which are assessed as on track. Five are already completed; five are behind schedule.
Viewed in the context of the recent drop in overdose mortality, the PRS updates would suggest that reducing drug-related deaths doesn’t actually require reducing access to drugs, but that’s probably beyond the scope of the ONDCP’s analysis.
The first objective for this goal was to reduce overdose deaths by 13 percent by 2025. The most recent Centers for Disease Control and Prevention data show a decrease of 16.9 percent, which according to the report is “[t]hanks in significant part to actions by the Administration.”
The second objective was to reduce prevalence of substance use disorders (SUD) specific to opioids, methamphetamine and cocaine by 25 percent.
The ONDCP attributed cocaine use disorder to 0.5 percent of the population in 2021, based on responses to the 2021 National Drug Use Survey. Which evolved between 2020 and 2021, and identifies different SUD by somewhat convoluted means, but the ONDCP doesn’t acknowledge non-problematic use of those substances and so approached use and SUD as the same thing. It attributed methamphetamine use disorder to 0.6 percent of the population, and opioid use disorder to 2 percent.
Per 2022 data, there’s been no change in baseline use of cocaine and meth. Opioid use increased to 2.2 percent, meaning “accelerated action” would be needed to finish on time.
While the previous goal applied to ages 12 and up, this goal of ensuring that “Prevention efforts are increased in the the United States,” refers to youth drinking and vaping.
The first objective was to get youth alcohol consumption, measured by past 30-day use, under 6.5 percent by 2025. Data show that between 2021 and 2022 the rate decreased from 7.2 percent to 6.8 percent, which put it on track.
The second objective was to reduce youth use of nicotine vapes by 15 percent by 2025. Data show that in 2021, around 7.6 percent of middle- and high-school students reported having vaped within the past month. In 2022 this rose to 9.4, but the target for 2025 was anything under 11.1, so ONDCP considers this objective already met and the 2022 increase doesn’t change that.
The first objective here was an 85-percent increase in the number of counties disproportionately affected by overdose that had at least one syringe service program (SSP). Data show that in 2020, 130 counties with high overdose death rates had at least one SSP; by 2022 this had increased to 180 counties, which was on track for the ONDCP goal of 241 counties by 2025.
The second objective was a 25-percent increase in SSP offering “some type of drug safety checking support service.” The 2025 target of 21.3 percent had already been met by 2021, but over the next year the number of SSP offering drug-checking services nearly doubled—2022 data show 46.7 percent of SSP met that criteria.
However, “some type” of drug-checking refers largely to fentanyl test strips, which are most useful to people who do not regularly use opioids. The more useful drug-checking service for people who do regularly use opioids—the population that SSP primarily serve—is on-site forensic analysis. This requires more expensive equipment, to which only a handful of SSP have access.
The first objective was a 100-percent increase in admissions to treatment facilities among people considered at high risk for overdose involving opioids, methamphetamine or cocaine. This doesn’t include methadone maintenance or outpatient buprenorphine prescriptions. In 2021, treatment facilities reported 637,589 admissions among people using primarily opioids, methamphetamine, cocaine or other “synthetics,” which was already about one-third short of the target for that year. In 2022 admissions dropped to 604,096.
The second objective was to ease the shortage of behavioral health providers by 70 percent. The PRS report finds that this been pretty steadily on track and is projected to stay that way.
The first objective here is to have at least 14 states operating a “recovery-ready workplace initiative” by 2025. The term refers to a Biden administration push for more equitable employment policies for workers with substance use disorder, which led to the creation of a national Recovery-Friendly Workplace Initiative in 2023. Data show this goal was met in 2022 with 16 states reporting a qualifying initiative, up from 13 in 2021.
The second objective was to increase the number peer-led recovery organizations to at least 194. This has been completed, as there were 232 as of 2022.
The third objective was to increase the number of recovery high schools to at least 47, which was on track with 45 operational as of 2022.
The fourth objective was to increase the number of collegiate recovery programs to at least 165, which was similarly on track with 149 as of 2022.
The fifth and final objective was to have at least 8,600 residential recovery programs operational by 2025. This too was on track as of 2022, with 7,957 programs.
Despite the extremely broad title, this goal had pretty narrow objectives. The first was to have 80 percent of drug courts complete equity and inclusion trainings by 2025. As of 2022 we were at 19 percent, considerably behind schedule. The PRS report attributes this to a combination of COVID-19 pandemic restrictions and bureaucratic restrictions, which it expects to resolve.
The second objective was a 100-percent increase in access to medications for opioid use disorder (MOUD) in federal Bureau of Prisons facilities, and a 50-percent increase for in state prisons and local jails.
The PRS report does not differentiate between access to methadone and buprenorphine, which have been shown to decrease overdose risk, and naltrexone—which has been shown to increase overdose risk, and of the three Food and Drug Administration-approved MOUD is by far the favorite among corrections departments. With that in mind, the ONDCP goal is on track for federal and state prisons.
“Currently, there is no single data source that can be used to track progress in increasing the percent of local jails offering MOUD,” the report states. “For illustrative purposes, [the figure below] shows the estimated percent of local jails offering MOUD in the United States from 2019 to 2022.”

The first objective for this goal was a 365-percent increase in the “number of targets identified in counternarcotics Executive Orders and related asset freezes and seizures made by law enforcement.” This refers to people and entities associated with transnational drug-trafficking organizations. Per the report, 46 had been identified by 2022, and the administration was on track to identify 96 by 2025.
The second objective was a 14-percent increase in the number of people convicted of felonies as a result of Drug Enforcement Administration investigations using data from the Financial Crimes Enforcement Network (FinCEN). Per the DEA, as of 2022 it had used FinCEN data in investigations that led to the convictions of 6,529 people. This surpassed the goal of 5,775 people convicted by 2025.
The third objective was to have at least 70 percent of the DEA’s active priority investigations “linked to the Sinaloa or Jalisco New Generation cartels, or their enablers.” This was also on track, at 62 percent in 2022.
The fourth objective was to decrease “potential production” of cocaine by 10 percent, and that of heroin by 30 percent.
“The United States Government is internally realigning responsibility for conducting illicit crop estimates. As a result of the change in responsibility, there will be a temporary gap in data for 2022 and 2023,” the report states in reference to both cocaine and heroin. “This gap in data does not reflect a change in priorities.”
Potential cocaine production was decreased only slightly between 2020 and 2021, but was projected to be on track as of 2021.
“[I]t is important to note that provisional estimates of drug overdose deaths involving cocaine for the 12-month period ending in July 2024 were 14.1 percent lower compared to a year prior,” the ONDCP added. “The Administration will continue its efforts to reduce the supply of cocaine.”
Heroin interdiction was not on track, but the ONDCP made the same statement verbatim for heroin-involved deaths.
The fifth objective was to have a total of at least 14 incident reports—like seizures or stopped shipments—involving fentanyl precursors from China or India. From 2021 to 2022 the number dropped from 11 to two, but the ONDCP notes that this data is voluntarily reported by other entities and as such is unreliable. And also that preliminary estimates for 2023 look a lot higher.
Source: https://filtermag.org/ondcp-national-drug-control-strategy/
Updated: Jan. 03, 2025, 12:02 p.m.|
By Julie Washington, cleveland.com
CLEVELAND, Ohio — Do music therapy and acupuncture help patients manage pain without opioids? University Hospitals will use a nearly $1.5 million federal grant to find out.
The grant allows UH to develop an Alternatives to Opioids program that educates caregivers about how music therapy and acupuncture can be used to decrease the use of opioids in the emergency department, the hospital system recently announced. The program also includes outpatient follow-up.
The goal is to reduce the use of prescribed opioids in emergency departments, UH said.
“When prescribing opioids there is always the potential for abuse,” said Dr. Kiran Faryar, director of research in the department of emergency medicine. “Data shows both music therapy and acupuncture improve pain and anxiety for patients with short-term and long-term pain. This will be an evidence-based technique we can offer patients without the potential risk of substance use disorder.”
UH’s comprehensive approach to combating the opioid crisis comes as the Centers for Disease Control and Prevention reported that 2023 drug overdose deaths in the United States decreased 3% from 2022. It was the first annual decrease in drug overdose deaths since 2018, the CDC said.
The trend was also seen in Ohio.
The number of people who died of drug overdoses in Ohio was 4,452 in 2023, a 9% decrease from the previous year, according to the state’s latest unintentional drug overdose report.
This was the second consecutive year of a decrease in deaths in Ohio. In 2022, overdose deaths declined by 5%, state officials said. Early data for 2024 suggest unintentional drug overdose deaths are falling even further this year.
In November, the state announced that agencies across Ohio would split $68.7 million in grants to combat opioid use and overdoses. The state is distributing the federal funding, part of the fourth round of the State Opioid and Stimulant Response grants, to support local organizations that offer prevention, harm reduction, treatment, and long-term recovery services for Ohioans struggling with an opioid or stimulant use disorder, the state announced.
Julie Washington covers healthcare for cleveland.com.
Source: https://www.cleveland.com/metro/2025/01/can-music-therapy-replace-opioids-for-pain-university-hospitals-investigates-with-15m-federal-grant.html
Powered by WordPress