Introduction
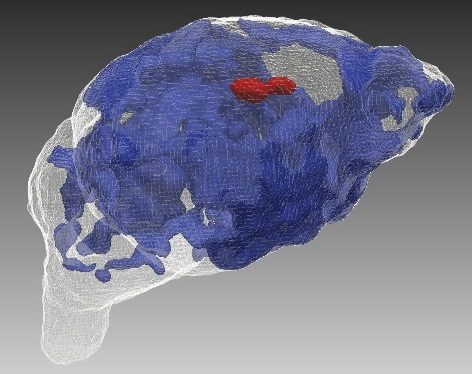
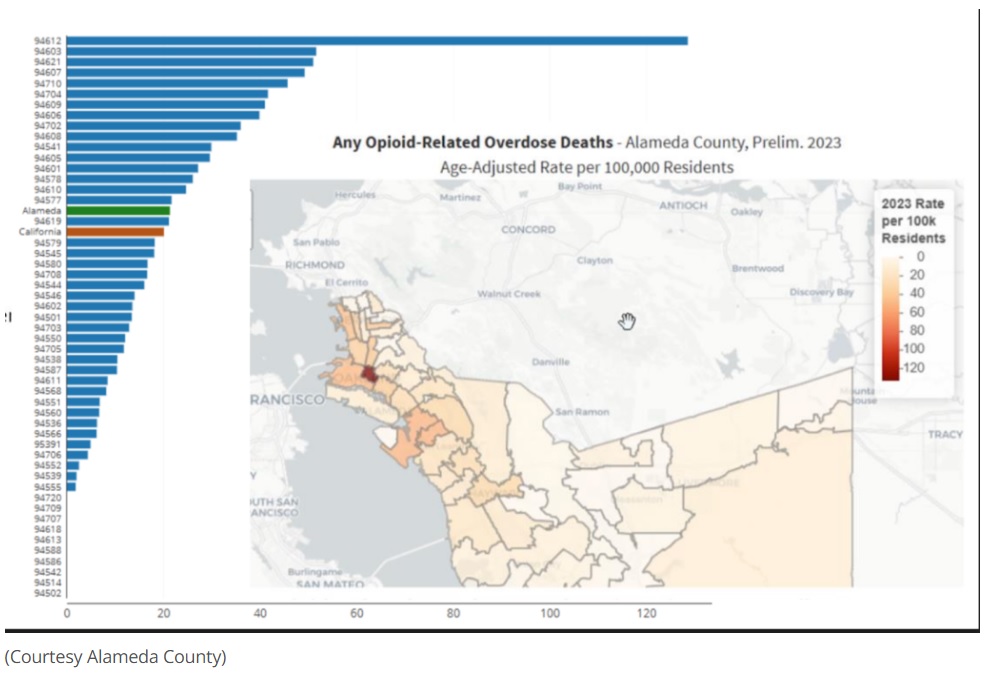
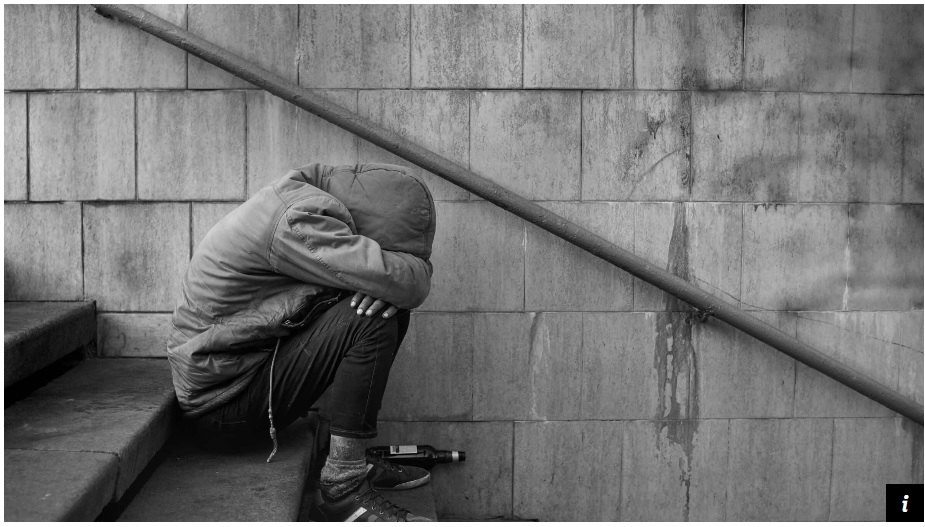
The opioid crisis continues to devastate the United States, with over 100,000 annual deaths linked to drug overdoses—75% involving opioids.1 Potent synthetic opioids like fentanyl exacerbate the crisis, often requiring multiple doses of naloxone to reverse an overdose. Naloxone, sold under the brand name Narcan, is a life-saving medication that quickly reverses opioid overdoses by blocking opioid receptors.2 With the surge in opioid-related deaths, harm reduction strategies like Narcan have become crucial tools in the fight against opioid addiction.2,3 Timely administration of Narcan can mean the difference between life and death, making widespread distribution and education on its use essential in combating the opioid crisis.
The COVID-19 pandemic intensified the opioid crisis, increasing substance use and overdose deaths due to isolation, economic instability, and disrupted healthcare services. Overdose death rates spiked nearly 30% between 2020 and 2021, underscoring the urgent need for accessible interventions.4 In March 2023, the US Food and Drug Administration (FDA) approved Narcan for over-the-counter (OTC) use, making it the first naloxone product available without a prescription. This landmark decision aimed to enhance harm reduction by expanding naloxone access to individuals at risk of overdose, their families, and communities.5
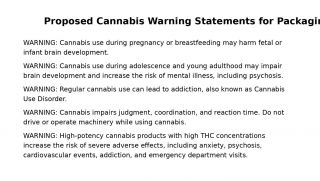
However, the OTC rollout has faced challenges. While major retailers now stock Narcan, the high price (around $45 per two-dose kit) remains a barrier.6 Rural and low-income pharmacies struggle with consistent availability, exacerbating disparities.7 Stigma surrounding opioid use and Narcan also persists, deterring some pharmacists from recommending or stocking it.8–10 Beyond access, awareness and confidence in using Narcan remain limited. Many potential users lack proper training, emphasizing the need for public education campaigns.11–13 Calls for naloxone training, similar to Cardiopulmonary Resuscitation (CPR) certification, highlight the importance of ensuring more people can effectively administer this life-saving intervention.14
The Robert Wood Johnson Foundation’s (RWJF) Culture of Health (COH) model provides a valuable framework for addressing these challenges.15 Developed through interdisciplinary consultation, evidence reviews, and stakeholder engagement, the COH model was designed to promote cross-sector collaboration, address social determinants of health, and foster equitable opportunities for well-being in all communities. It is particularly relevant to the opioid crisis, where stigma, fragmented systems, and entrenched inequities impede progress. Since its introduction in 2015, the COH model has been widely applied in public health, community development, and health equity efforts, demonstrating its utility as both a conceptual and practical guide for systemic change.16,17
While models such as the Social Ecological Model (SEM) and Social and Behavior Change Communication (SBCC) approaches emphasize the importance of multilevel interventions and sustainable behavior change, they often remain abstract and narrowly focused on programmatic strategies.18,19 In contrast, the COH model operationalizes these principles into a tangible, systems-level blueprint for driving long-term societal transformation. Applying the COH model to overdose prevention offers a comprehensive approach for shifting societal values, strengthening healthcare and community systems, and promoting resilience.
The four pillars of the COH model, (1) making health a shared value, (2) fostering cross-sector collaboration, (3) ensuring equitable healthcare access, and (4) transforming healthcare systems, are deeply interconnected rather than mutually exclusive. Some thematic overlap across the pillars is therefore expected and reflects real-world dynamics where key stakeholders, including pharmacies, healthcare providers, law enforcement, and community organizations, intersect across multiple strategies to address opioid overdose prevention. Drawing upon this framework, this paper examines how the COH model can guide the translation of the FDA’s Narcan ruling into meaningful public health impact. It explores challenges, opportunities, and evidence-based interventions aligned with each pillar, offering strategic insights for overcoming stigma, expanding naloxone distribution, promoting cross-sector partnerships, and embedding harm reduction within healthcare and community systems.
Purpose and Significance
Building on this framework, this paper applies the COH model to examine how the four pillars—making health a shared value, fostering cross-sector collaboration, ensuring equitable access, and transforming healthcare systems—can guide the translation of the FDA’s over-the-counter approval of Narcan into sustained public health impact.
By examining each pillar, this paper identifies key challenges, opportunities, and evidence-based strategies for creating a culture of health that prioritizes opioid overdose prevention and recovery. It highlights how stigma, access disparities, and systemic barriers can be overcome through targeted interventions, collaboration across sectors, and an integrated approach to harm reduction and treatment.
The significance of this work lies in its potential to guide stakeholders in translating the FDA ruling into actionable and sustainable solutions. The COH model provides a unique lens through which to address the structural inequities and social determinants of health that underlie the opioid crisis. By offering a comprehensive roadmap for building healthier, more equitable communities, this paper contributes to the broader public health effort to reduce overdose deaths and support individuals on their path to recovery. Given the interconnectedness of the COH pillars, some thematic overlap is expected, particularly regarding key strategies such as stigma reduction, cross-sector collaboration, and harm reduction integration, which span multiple domains of action.
Pillar 1: Making the Prevention of Opioid Overdose Deaths a Shared Value
The first pillar of the COH model, making health a shared value, emphasizes the need for a collective mindset in addressing public health crises.20 Preventing opioid overdose deaths requires not only access to Narcan but also a cultural shift where opioid overdose is seen as a community issue rather than an individual failing. Overcoming stigma surrounding opioid use disorder (OUD) is central to fostering shared responsibility.21
Addressing Stigma in Communities and Pharmacies
Stigma remains a major barrier to naloxone access. Many individuals hesitate to seek naloxone due to fear of being judged, while some pharmacists are reluctant to dispense it, believing it enables risky opioid use.22 Studies show that low-income and rural pharmacies are less likely to stock naloxone, limiting access in the very communities that need it most.23
However, promising initiatives demonstrate that stigma reduction can improve naloxone uptake. For example, in San Francisco, robust harm reduction messaging and naloxone distribution programs have helped normalize overdose prevention.24 These initiatives illustrate how treating overdose as a medical emergency rather than a moral failure can encourage individuals to seek naloxone without fear.25
The Role of Harm Reduction
Harm reduction is a crucial framework in changing societal views about opioid use. It emphasizes the importance of helping individuals where they are without judgment or discrimination.26 Harm reduction approaches, like the distribution of Narcan, aim to reduce the immediate harm caused by opioid use while acknowledging that recovery is a long-term process.25 Naloxone is increasingly recognized as a first-aid tool that can save lives in the same way as Cardio-Pulmonary Resuscitation (CPR) or an EpiPen does, shifting public perception of overdose response from an individual issue to a community responsibility.9
For example, in Massachusetts, a statewide overdose education and naloxone distribution program trained community members and law enforcement in Narcan administration.27 Thousands of overdoses have been reversed through these efforts, proving that equipping communities with the right tools can save lives.28
Shifting the Law Enforcement Perspective
Law enforcement officers are often the first responders to overdose emergencies, and their role in administering Narcan is pivotal. However, some police departments have been slow to adopt naloxone due to concerns about enabling drug use.12
Yet, success stories like those in Seattle, Washington, have demonstrated how law enforcement can become part of the solution.29 By adopting harm reduction principles, the Seattle Police Department began equipping officers with naloxone, saving over 100 lives in just one year.29 Changing police training to prioritize harm reduction over punitive measures can help officers view overdose prevention as part of their public duty rather than an enforcement challenge.30
The Role of Public Education
Public education campaigns are crucial in making naloxone use a shared responsibility. Initiatives in Rhode Island and Ohio have successfully increased community engagement by distributing naloxone kits alongside instructional materials.31,32 These efforts emphasize that anyone—a family member, friend, or bystander—can intervene in an overdose and save a life.
In summary, the first pillar of the COH model calls for a cultural shift in how opioid overdose prevention is perceived. Reducing stigma, fostering harm reduction, engaging law enforcement, and expanding public education are essential strategies in making naloxone access a shared value. Success stories from community pharmacy programs, law enforcement adoption, and public health initiatives underscore the importance of collaboration in changing societal attitudes. By making overdose prevention a collective responsibility, communities can create a culture of health that prioritizes saving lives.
Pillar 2: Fostering Cross-Sector Collaborations to Improve the Well-Being of People Affected by Opioid Overdose
The second pillar of the COH model emphasizes the importance of fostering cross-sector collaborations to address complex public health challenges.15 In the case of opioid overdose prevention, cross-sector collaboration is essential to ensure that individuals affected by OUD receive not only immediate overdose reversal via Narcan but also access to long-term treatment and recovery options. The FDA’s approval of OTC Narcan has opened new avenues for collaboration, particularly between traditional healthcare settings and community-based organizations that can distribute and educate the public about naloxone.5 However, challenges remain, in effectively coordinating these efforts across different sectors to maximize impact.33
Pharmacies and Public Health Agencies: A Crucial Partnership
Pharmacies play a pivotal role in the distribution of Narcan, as they are often the most accessible healthcare providers in many communities.34 However, their effectiveness depends on partnerships with public health agencies to address stigma, insurance coverage gaps, and disparities in access. Some community pharmacies work with local health departments to ensure naloxone availability, particularly in high-risk areas.35 For example, in Ohio, collaboration between pharmacies and the state health department has expanded naloxone distribution and pharmacist education.35,36
However, many rural and low-income urban pharmacies struggle to stock naloxone due to financial constraints. The state of Massachusetts has addressed this by funding pharmacy naloxone programs and mandating availability. Expanding such initiatives to other states could further reduce access barriers.37
Engaging Law Enforcement in Overdose Prevention
Law enforcement officers are often first responders to overdoses, making their involvement crucial.33 However, law enforcement participation in overdose prevention has been uneven due to concerns about enabling drug use and a lack of clarity on the role of harm reduction in public safety. Nevertheless, successful cross-sector collaborations between law enforcement and public health advocates have demonstrated the potential for law enforcement officers to play a vital role in overdose prevention.33,38
One example of effective collaboration is the Law Enforcement Assisted Diversion (LEAD) program, implemented in multiple cities, allowing officers to divert individuals with substance use disorders to treatment rather than jail.38 In Seattle, Washington, this approach has led to fewer drug-related arrests and greater engagement in recovery services.38
Similarly, Ohio police officers carrying naloxone have reversed thousands of overdoses with support from local health agencies providing training and supplies. Expanding naloxone training for law enforcement officers and integrating harm reduction into policing can further strengthen overdose response efforts.39
Hospitals and Community-Based Organizations: Bridging the Treatment Gap
Hospitals are another key player in overdose prevention, as they are often the first point of contact for individuals following a non-fatal overdose.40 However, ensuring that individuals receive follow-up care and access to long-term treatment remains a significant challenge. Cross-sector collaboration between hospitals and community-based organizations can help bridge this gap.41
For example, the “Warm Handoff” model, implemented in states like Pennsylvania and Rhode Island, involves connecting individuals who have experienced an overdose with peer recovery specialists before they are discharged from the hospital.42 In Rhode Island, this model has resulted in a significant increase in treatment engagement among individuals who have experienced a non-fatal overdose.43
Additionally, some hospitals now include naloxone kits and harm reduction education in discharge protocols. Expanding partnerships between hospitals and harm reduction organizations in the community can improve long-term outcomes for individuals at high risk of overdose.44
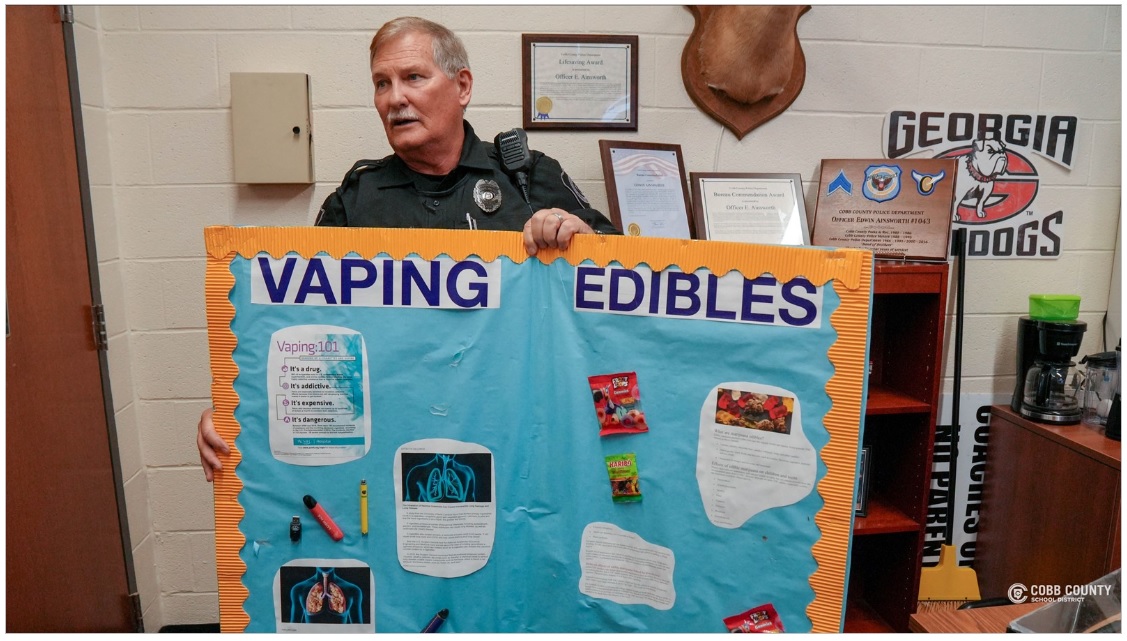
Schools and Educational Institutions: Expanding Naloxone Training
Schools have an important role to play in overdose prevention, particularly in areas where opioid use is prevalent among youth.45 Cross-sector collaborations between schools, public health agencies, and harm reduction organizations can help ensure that naloxone training is integrated into educational curricula and that students are equipped with the knowledge to respond to an overdose.46 In New Jersey, the Department of Education partnered with local health agencies to provide naloxone training to students and staff, increasing awareness and preparedness.47 Expanding similar programs nationwide could further strengthen community overdose response.48
In summary, fostering cross-sector collaboration is essential for expanding Narcan use and improving overdose prevention. Pharmacies, public health agencies, law enforcement, hospitals, and schools each play a critical role. Programs like LEAD, Warm Handoff, and school-based naloxone training demonstrate the effectiveness of collaboration in saving lives and promoting harm reduction. However, challenges remain, particularly in addressing disparities in naloxone access and shifting attitudes toward harm reduction. Continued investment in cross-sector partnerships is necessary to ensure that naloxone reaches those who need it most.
Pillar 3: Creating Healthier Communities by Investing in Efforts to Ensure Equitable Access to Narcan
The third pillar of the COH model emphasizes creating healthier communities by advancing policies and practices that promote well-being for all.15 Equitable access to life-saving interventions like Narcan is central to addressing the opioid crisis in the United States. While Narcan has proven to reduce opioid overdose deaths, barriers to access persist, especially among vulnerable populations.6,8 Addressing these barriers is essential for building healthier, more resilient communities.
Insurance Coverage and Affordability Barriers
Despite the FDA’s approval of over-the-counter Narcan, cost remains a significant barrier, particularly for those without insurance.49 Medicaid and Medicare generally cover naloxone, but private insurance coverage is inconsistent, and out-of-pocket costs can exceed $120 for a single box, making it unaffordable for low-income individuals and families in areas most impacted by the opioid epidemic.50
Many pharmacies in low-income communities do not carry Narcan due to limited demand, driven partly by high costs and lack of insurance coverage.10 Some states, like New York, have programs such as the Naloxone Co-payment Assistance Program (N-CAP), which covers up to $40 of co-payments for naloxone prescriptions.51 However, uninsured individuals still face significant challenges. Expanding public funding and mandating insurance coverage for naloxone could reduce these disparities.52
Geographic Disparities in Naloxone Access
Naloxone availability also varies significantly by region, with rural and low-income urban areas facing the greatest challenges.53 Pharmacies in these regions are less likely to stock naloxone due to lower demand and limited resources, leaving high-risk communities without access to this life-saving medication.23
To address these disparities, some states have implemented standing orders allowing pharmacies to dispense naloxone without a prescription.54 In Massachusetts, a statewide standing order has substantially increased naloxone distribution, particularly in rural areas.55 Harm reduction organizations have also stepped in to fill gaps in access.25 For instance, in West Virginia, harm reduction programs have distributed thousands of naloxone kits to rural communities, reducing overdose deaths.56
The Role of Independent and Chain Pharmacies
A stark contrast exists between independent and chain pharmacies in naloxone availability. Independent pharmacies, especially in rural areas, are less likely to stock naloxone due to financial constraints and concerns about serving individuals who use drugs.57 In contrast, chain pharmacies like CVS and Walgreens are more likely to stock naloxone and have policies in place to ensure availability.58
CVS, for example, launched a public education campaign to increase awareness of Narcan’s availability and its role in saving lives.59 However, independent pharmacies in underserved areas still require targeted support, including financial incentives and education programs, to address these disparities and ensure naloxone reaches communities in need.60
Overcoming Stigma and Promoting a Culture of Health
Stigma remains one of the most significant barriers to naloxone access. Many individuals who use opioids hesitate to seek naloxone out of fear of judgment or being labeled as drug users. This stigma extends to healthcare providers, pharmacists, and law enforcement officials, some of whom are reluctant to stock or distribute naloxone due to misconceptions that it enables risky opioid use.21
Shifting public perceptions is critical to overcoming these barriers. Public health campaigns, like California’s “Know Overdose” initiative, educate communities about naloxone’s role as a harm reduction tool that saves lives.61 These campaigns emphasize that opioid overdoses are medical emergencies requiring immediate intervention, similar to heart attacks or strokes. By changing attitudes, such initiatives help normalize naloxone use and encourage greater distribution in communities affected by the opioid crisis.62
Success Stories: Expanding Naloxone Access Through Public Policy
Several states and cities have successfully expanded naloxone access through innovative public policy initiatives. In Rhode Island, the Department of Health allows community organizations to distribute naloxone directly to individuals without requiring them to visit a pharmacy.43 This approach has been particularly effective in reaching homeless individuals and those living in poverty.
Similarly, Illinois runs a statewide program providing free naloxone kits to people at risk of overdose and their loved ones. These kits are distributed through a network of healthcare providers, harm reduction groups, and community organizations, ensuring naloxone reaches those who need it most.63
In Philadelphia, the city’s health department partnered with local businesses to distribute naloxone at convenience stores, libraries, and recreation centers, improving access in neighborhoods with high overdose rates. Such efforts demonstrate the potential for innovative strategies to reduce opioid-related deaths by ensuring naloxone is readily available in underserved communities.64 Similarly, in Minnesota, public health officials have launched Narcan vending machines in Minneapolis, ensuring 24/7 access to the medication in high-risk areas, further demonstrating how innovative distribution strategies can improve equitable naloxone access.65
In summary, creating healthier communities through equitable access to Narcan requires addressing cost, insurance coverage, and geographic disparities while reducing stigma. Public policy initiatives, partnerships between pharmacies and public health agencies, and public education campaigns are all essential components. Success stories from states like Massachusetts, Rhode Island, and Illinois highlight the impact of these efforts, but continued investment is needed to expand access to all at-risk populations. By prioritizing equitable access to naloxone, communities can take significant steps toward reducing overdose deaths and improving public health outcomes.
Pillar 4: Transforming Health and Healthcare Systems for Treatment of Opioid Use Disorder
The fourth pillar of the COH model emphasizes integrating healthcare and public health services to ensure equitable access to quality, affordable care. This is particularly critical for addressing OUD, which requires transforming healthcare systems to deliver comprehensive, evidence-based treatment that includes harm reduction, medication-assisted treatment (MAT), and long-term recovery support.66 The FDA’s approval of over-the-counter Narcan is a step in this direction, but systemic changes are needed to address the broader opioid crisis.66
Integrating Harm Reduction Into Healthcare Systems
Harm reduction, including naloxone distribution, is central to OUD care. However, healthcare systems must go beyond providing naloxone to integrate harm reduction into routine care. Hospitals play a crucial role through initiatives like “warm handoffs”, where overdose patients in emergency departments (EDs) are connected with addiction specialists or recovery services before discharge.67 This approach ensures follow-up care, including MAT and access to harm reduction tools such as fentanyl test strips.53,68
In Rhode Island, hospitals have integrated naloxone distribution into discharge protocols for OUD patients, reducing repeat overdoses and increasing engagement in recovery services. Such efforts demonstrate how transforming hospital protocols can embed harm reduction as a standard part of care.67,69
Expanding Access to Medication-Assisted Treatment (MAT)
MAT, which combines medications like methadone or buprenorphine with behavioral therapies, is one of the most effective treatments for OUD. However, access to MAT is uneven, particularly in rural and underserved areas.53 Telemedicine has emerged as a valuable solution, especially during the COVID-19 pandemic when regulatory changes allowed for remote MAT delivery.70 Permanently adopting telehealth flexibilities can further expand MAT access for those in areas with limited healthcare infrastructure.
Community-based pharmacies have also begun dispensing buprenorphine, providing additional access points for individuals who lack specialized addiction treatment centers. This model increases accessibility and helps normalize OUD treatment within the broader healthcare system, reducing stigma.71
Training Healthcare Providers to Address OUD
A significant barrier to improving OUD treatment is the lack of provider training. Many doctors, nurses, and pharmacists receive little education on substance use disorders, leading to missed intervention opportunities.72 States like Massachusetts have started addressing this gap by requiring prescribers to complete training on opioid safety, naloxone use, and MAT referrals.73 Expanding such requirements to include all healthcare providers, including behavioral and allied health professionals, would strengthen the workforce’s capacity to address OUD.74
Healthcare systems can also leverage online training modules and virtual workshops to keep providers updated on evidence-based practices.75 By investing in training, healthcare systems can create a more informed and effective workforce capable of meeting the needs of individuals with OUD.
Using Data to Drive Systemic Change
Leveraging data is essential for transforming healthcare systems to address OUD. Electronic health records (EHRs) and claims data can identify high-risk patients and enable targeted interventions. For example, pharmacies can track opioid prescriptions and provide naloxone or MAT to patients identified as at-risk.76
Public health agencies can collaborate with healthcare systems to implement data-driven strategies. In Pennsylvania, the Prescription Drug Monitoring Program (PDMP) has been used to track prescriptions, reduce overprescribing, and identify individuals at risk of overdose.76 By integrating PDMP data with public health initiatives, Pennsylvania has reduced opioid-related deaths and improved access to treatment.76,77
By combining harm reduction, MAT expansion, provider training, and data-driven strategies, healthcare systems can play a pivotal role in addressing the opioid crisis and supporting individuals with OUD.78
Discussion
The application of the four pillars of the COH model provides significant insights into the multifaceted strategies needed to address the opioid crisis through the wider use of Narcan. Each pillar emphasizes different dimensions of collaboration, equity, and system transformation, all of which are essential for reducing opioid overdose deaths and supporting individuals with OUD. Notably, success stories across different states demonstrate how the four pillars can operate synergistically to improve overdose outcomes. In Massachusetts and Rhode Island, comprehensive strategies integrating public health, healthcare, and community partners have expanded naloxone access, reduced stigma, and improved care transitions. In San Francisco, robust harm reduction messaging and community-based naloxone distribution initiatives have shifted cultural perceptions. Similarly, Ohio and Seattle, Washington, have demonstrated the importance of law enforcement engagement and cross-sector partnerships in supporting overdose prevention and recovery efforts. These examples illustrate that while each pillar offers distinct insights, their real-world application often occurs in combination, reinforcing the need for integrated, place-based approaches to building a Culture of Health. At the same time, each pillar addresses a unique dimension of systemic change: making health a shared value fosters societal norms that reduce stigma; cross-sector collaboration mobilizes diverse resources and leadership; equitable access ensures that life-saving interventions reach marginalized populations; and transforming healthcare systems embeds harm reduction and recovery support into clinical practice. Recognizing the distinct role of each pillar is critical to designing comprehensive and sustainable public health strategies to address the opioid crisis.
Summary of Insights and Takeaways from the Four Pillars
Pillar 1 emphasizes making opioid overdose prevention a shared value by overcoming stigma and fostering community-wide responsibility. Stigma in pharmacies and law enforcement discourages individuals from seeking naloxone.17,20 Successful harm reduction efforts in San Francisco and Massachusetts demonstrate that community support and education can normalize naloxone as a life-saving intervention, akin to other emergency medical tools.9,24,27
Pillar 2 underscores the importance of cross-sector collaborations in promoting Narcan’s use. Partnerships among pharmacies, law enforcement, hospitals, and community organizations have proven effective in programs like the LEAD program and hospital-based naloxone distribution. These collaborations increase access to timely overdose interventions and long-term treatment.38
Pillar 3 highlights the need to address economic and geographic barriers to Narcan access in rural and low-income communities. Initiatives in Rhode Island, New York, and Massachusetts have improved access by reducing costs and promoting community collaborations. Addressing disparities and ensuring pharmacies stock naloxone are essential to saving lives.43,51,54,55
Pillar 4 focuses on transforming healthcare systems to integrate harm reduction and MAT. Telemedicine has expanded MAT access in underserved areas, while hospital “warm handoff” programs connect overdose survivors to treatment. Systemic changes are vital for delivering comprehensive, patient-centered care for individuals with OUD.53,66–70
Implications for Practice
The insights gained from applying the COH model to opioid overdose prevention highlight several critical implications for practice across different sectors. For pharmacies, both chain and independent, there is a need to ensure that naloxone is readily available and affordable. Pharmacies should collaborate with public health departments37 to promote naloxone access, provide patient counseling, and participate in community education campaigns to reduce stigma.
For healthcare providers, including hospitals, clinics, and primary care practices, integrating harm reduction strategies like naloxone distribution and MAT into routine care is essential. Hospitals should implement protocols for overdose patients that include naloxone distribution and referrals to recovery services upon discharge.66,68,70
For law enforcement, adopting harm reduction principles and collaborating with healthcare providers and community organizations, as seen in LEAD programs, can help officers view overdose prevention as part of their public safety duties.38
Families and communities also play a key role in overdose prevention by learning how to use naloxone and supporting loved ones struggling with OUD. Public education campaigns should target families and at-risk communities to increase awareness and reduce stigma.31,32
Implications for Policy
Policymakers should prioritize expanding insurance coverage for naloxone, including making it available at no cost for uninsured individuals. States should consider mandating the stocking of naloxone in all pharmacies, particularly in high-risk areas, and provide financial support to independent pharmacies to ensure affordability.14,33,37,57 Additionally, telemedicine should be made a permanent option for MAT to improve access in underserved regions.70
Implications for Future Research
Further research is needed to evaluate the long-term effectiveness of cross-sector collaborations in reducing opioid overdose deaths. Additionally, studies should explore the impact of public education campaigns on reducing stigma and increasing naloxone usage. Understanding the barriers to naloxone access in rural and low-income areas will also be critical to developing more targeted interventions.53
In summary, addressing the opioid crisis requires coordinated efforts across all sectors of society. By applying the COH model’s four pillars—shared values, cross-sector collaboration, equitable access, and healthcare system transformation—communities can create a sustainable framework for reducing overdose deaths and supporting long-term recovery for individuals with Opioid Use Disorder.15,17,20
Conclusion
The US opioid epidemic remains one of the most urgent public health challenges of our time, demanding a shift from conventional healthcare interventions to broader system-level and cultural change. The FDA’s approval of over-the-counter Narcan represents a pivotal milestone, but its potential will be realized only through strategic efforts to make naloxone truly accessible, affordable, and normalized within communities. Applying the RWJF Culture of Health (COH) model, this paper presents a comprehensive roadmap for advancing harm reduction strategies, promoting equitable access, and integrating systemic reforms to combat opioid overdose deaths.
Evidence reviewed in this paper demonstrates that stigma remains a profound barrier to naloxone access and utilization, deterring both individuals and healthcare providers. Community-based naloxone distribution programs and public education campaigns, such as those implemented in San Francisco, Rhode Island, and Philadelphia, offer powerful models for increasing public uptake and saving lives. Nevertheless, challenges persist: Narcan’s price point, geographic disparities in availability, and limited public awareness continue to undermine the promise of OTC access. While national policy efforts have prioritized naloxone expansion, the full potential of these initiatives will depend on addressing these systemic barriers through multi-sector collaboration and sustained public health investment.
Ultimately, addressing the opioid crisis demands both urgent action and long-term cultural change. The COH model provides a guiding framework for engaging stakeholders across healthcare, public health, law enforcement, and community organizations to create a system where overdose prevention is a shared value and recovery pathways are accessible to all. Though uncertainties remain about how quickly OTC Narcan adoption will scale, the collective lessons from harm reduction and cross-sector collaboration are clear: building healthier, more resilient communities requires persistence, innovation, and a commitment to health equity.
Looking ahead, sustained and coordinated action across sectors will be critical to achieving the systemic and cultural changes needed to end the opioid epidemic. By fostering a culture of health that embraces harm reduction, advances equitable access, and transforms healthcare systems, we can help turn the tide on the opioid epidemic. The journey toward a healthier and more compassionate society will require sustained collaboration, innovation, and a commitment to addressing the social and structural determinants that perpetuate opioid-related harm. With deliberate and coordinated action, we can build a future where life-saving interventions like Narcan are universally accessible, and every individual has a fair opportunity for recovery and wellness.