From: drug-watch-international@googlegroups.com On Behalf Of Maggie Petito mlp3@starpower.net
Sent: 08 January 2026 11:46
According to his captors, the Venezuelan president is not a mere cartel boss. He is the most powerful drug trafficker ever to face justice
by London Daily Telegraph – Colin Freeman – 07 January 2026
(The following article is derived from a previous article by a Mr. Maltz, U.S. DEA, Ret)
For customs agents at Paris’s Charles de Gaulle airport, the haul was like nothing they had ever seen. Packed into 30 suitcases on an airliner from Venezuela’s Maiquetia airport was 1.3 tonnes of pure cocaine – the biggest airport seizure in French history. It was, however, clearly no routine “drug mule” operation. Whoever had got such a huge amount through Venezuelan airport security must surely have had inside help. According to an indictment unsealed in a New York courtroom this week, that help went well beyond a few corrupt baggage handlers. Instead, the ultimate “insider” was Venezuelan president, Nicolás Maduro, who appeared in court on Monday, accused of drug trafficking on a mammoth scale.
Maduro, prosecutors allege, “abused” his public roles for over 25 years, and “partnered with his co-conspirators to use his illegally obtained authority… to transport thousands of tonnes of cocaine” from airports, airstrips and ports run by conniving regime officials to America and Europe.
The Department of Justice’s (DOJ) indictment says that following the Paris airport seizure in 2013, Maduro’s regime arrested dozens of local officials as a “cover up”. However, behind the scenes, he held a panicked summit with Diosdado Cabello, Venezuela’s current interior minister, and Hugo Carvajal, the former head of military intelligence.

A member of the National Guard watches over 2.6 tonnes of cocaine seized in Zulia, Venezuela, in 2013 Credit: Jimmy Pirela/AFP/Getty Images
“During the meeting, Maduro told Cabello and Carvajal that they should not have used the airport for drug trafficking after the 2006 seizure in Mexico [where five tonnes of cocaine were discovered in a commercial plane arriving from Venezuela], and that they should instead use other well-established drug routes. “Shortly thereafter, Maduro authorised the arrests of certain Venezuelan military officials in an effort to divert public and law enforcement scrutiny away from the shipment and its cover up.”
‘Cartel of the Suns’
Inside details of the Paris airport bust emerged after Maduro was snatched from Caracas by US commandos on Saturday, along with his wife, Cilia Flores, who faces similar charges.
Both have pleaded not guilty, with the erstwhile Venezuelan leader declaring himself a “prisoner of war” when he stood in the dock on Monday.
Yet if US officials are to be believed, he is possibly the most powerful trafficker ever to face justice – not a mere cartel boss, like Colombia’s Pablo Escobar or Mexico’s Joaquín “El Chapo” Guzmán, but the serving head of a nation state, who used its levers of power to flood the West with cocaine. The DOJ’s indictment alleges that he heads the “Cartel of the Suns”, a military-run trafficking group, so named because of the sun-shaped stars on Venezuelan generals’ epaulettes.
Whether US prosecutors can prove their claims is another matter. Doubts have already been raised, for example, over whether the Cartel of the Suns is a genuine syndicate in the manner of Escobar’s or Guzmán’s. Some analysts claim it is nothing more than Venezuelan slang for any official figure suspected of corruption. And while Trump has called Maduro a drug “kingpin”, the courtroom battle will come down to whether lawyers are able to marshal solid, detailed evidence to convince any judge and jury of his alleged crimes.
Nonetheless, the indictment cites multiple instances of Maduro directly facilitating the drug trade, from organising diplomatic passports for known gangsters to hosting cocaine trafficking paramilitaries at his presidential palace.
A narco-state
Irrespective of his personal culpability, most analysts also agree that under Maduro and his predecessor, Hugo Chavez, Venezuela has become a classic narco-state – a lawless, gun-ruled country, where drugs are one of the few ways to make money.
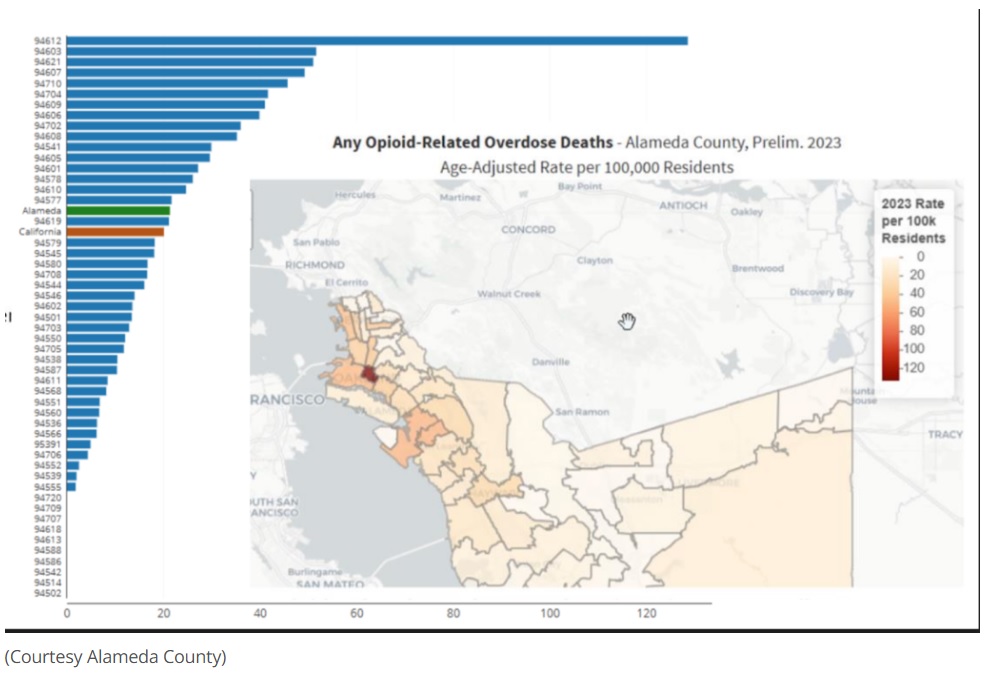
Law enforcement officials say it is now a major hub for cocaine from neighbouring Colombia, with its position on Latin America’s north east coastline making it a perfect launch spot for shipping to Europe. According to UN estimates, 40 per cent of the class A drug that reaches Europe passes through Venezuelan borders first.
In fairness, the country was a smugglers’ paradise even before Chavez took over in 1999. With a porous 1,500-mile border with Colombia – where most cocaine is produced – and a long Caribbean coastline, plus lots of dense, remote jungles, it has long been a place that is both easy to hide in and hard to police. At the same time, its modern networks of roads and ports – built with Venezuela’s oil wealth in stabler times – make it easy for gangs to transit contraband quickly.
According to Insight Crime, which reports extensively on Latin America’s drug trade, Cosa Nostra mafia clans also settled there in decades gone by as part of a post-war wave of Italian immigration. From the 1980s, they embraced the cocaine trade, which soon also began corrupting the Venezuelan government.
Things got dramatically worse, however, under Chavez’s hardline socialist regime. A ferocious critic of the “imperialist” US, he took the view that Venezuela was not to blame for the cocaine habits of wealthy North Americans. In 2005, he expelled the US Drug Enforcement Administration (DEA) from Venezuela, claiming that its “war on drugs” was an excuse to spy on his regime.
Western officials, however, linked the expulsion to his partnership with Colombia’s Left-wing FARC paramilitary group, which paid huge bribes to traffic cocaine through Venezuelan territory.
‘Cocaine Air’
As Chavez’s socialist policies gradually wrecked the economy, smuggling profits became key to regime survival, with ministers, the security services and powerful street gangs all involved.
Named in the US indictment alongside Maduro, for example, is Hector Rusthenford Guerrero Flores, the leader of Venezuela’s notorious Tren de Aragua gang. The indictment claims that heavily armed Tren de Aragua footsoldiers would escort cocaine shipments to airports and secret airstrips.
So emboldened were Venezuela’s traffickers that they would even commandeer old airliners to export their product, in what was dubbed “Cocaine Air”. One prominent case cited in the indictment was in 2006, when a DC9 airliner carrying 5.5 tonnes of cocaine was seized in Mexico. It had taken off from the presidential runway at Maiquetia airport, which lies just outside Caracas.
The shipment is thought to have been organised by Walid Makled, a Venezuelan businessman later jailed for other trafficking crimes. During his trial, he declared, “All my business associates are generals.”
Maduro is also accused of selling diplomatic passports to known traffickers when he served as foreign minister. This, the indictment says, was to help channel bags of cash from drug sales in Mexico back into Venezuela, using diplomatic cover to stop the bags from being searched.
“On these occasions, Maduro called the Venezuelan embassy in Mexico to advise that a diplomatic mission would be arriving by private plane,” the indictment says. “Then, while the traffickers met with the Venezuelan ambassador to Mexico under the auspices of a diplomatic mission from Maduro, their plane was loaded with the drug proceeds. The plane would then return to Venezuela under diplomatic cover.”
Trafficking product through Africa
Drug enforcement experts believe that “Cocaine Air” was only possible because Venezuela’s traffickers had access to proper airports, where full-size airliners could take off and land. The larger planes also extended the traffickers’ reach, allowing them to open up new smuggling routes to West Africa, where product would be warehoused before being shipped to Europe.
In 2009, a burned-out Venezuelan Boeing 727 was found in a remote area of Mali, having apparently ferried up to 10 tonnes of cocaine. Venezuelan smugglers were also flying cocaine into the bankrupt west African nations of Guinea and Guinea Bissau. Both were burgeoning narco-states at the time, with cocaine cartels having bought up almost their entire governments.
The US first publicly accused Maduro of trafficking in 2020, when he was named in an indictment along with Carvajal and Cabello. The latest indictment expands the allegations against Maduro and also accuses him of partnering with “narco-terrorists” including FARC, Mexico’s Sinaloa and Los Zetas cartels, and the Tren de Aragua gang.
Among the five others named in the indictment is Maduro’s son, Nicolás Ernesto Maduro Guerra, who is accused of flying drug packages to Margarita Island, a known smuggling haunt off Venezuela’s northern coast. In 2020, Guerra also allegedly met with FARC guerrillas in Colombia to discuss smuggling “large quantities of cocaine and weapons into the United States over the course of the next six years”.
The indictment also mentions the notorious “narco-nephews” case, in which two nephews of Maduro’s wife were arrested on drug trafficking charges by undercover DEA agents in Haiti in 2015.
The pair, who flew into Haiti on a plane carrying 800 kilos of cocaine, were jailed for 18 years in New York in 2017.
Former allies turning against Maduro?
Among those who will be following Maduro’s trial closely is retired narcotics agent, Derek Maltz, who headed the DEA’s Special Operations Division from 2005 to 2014. He helped lead the team that went on to capture “El Chapo” 12 years ago and also monitored Venezuela’s rising prominence as a narco-hub. He believes the US authorities would not have moved on Maduro without building up a strong case first.
“They have a huge amount of experience in putting these kinds of cases together,” he says. “In my experience, these investigations usually rely on high-level confidential sources, which are then corroborated with other evidence.”
Maltz adds the prosecution could well draw on testimony from fellow Maduro regime members, several of whom have already been arrested by the US over the years, and who might cooperate in return for reduced sentences.
One possible figure is Carvajal, who was arrested in Spain in 2021, and sentenced to life imprisonment on trafficking charges in the US last June. He is now tipped as a possible star witness, having reportedly written a letter to President Donald Trump last month in which he said he was willing to testify.
Maduro’s son, Nicolás Ernesto Maduro Guerra, is accused of flying drug packages to Margarita Island Credit: Leonardo Fernandez Viloria/Reuters
Maltz compares it to the groundbreaking 1990s prosecution of New York mob boss, John Gotti – dramatised in the 1994 film, Getting Gotti, in which a former associate, Sammy “The Bull” Gravano, gave evidence in return for leniency for his own crimes.
“Carvajal is thought to have set up a lot of the smuggling infrastructure, running operations under both Maduro and Chavez,” Maltz says. “A guy like that could be very useful. These kinds of people can also usually produce corroborative evidence, whether it’s phone call records, emails, bank account details or whatever.”
Given that Maduro and his wife will be able to afford America’s best defence lawyers, it remains to be seen whether evidence will secure convictions. But for Maltz, the prospect of seeing Venezuela’s role in the drug trade aired in a courtroom will be welcome in itself.
“When I took over the Special Operations Division in 2005, it came to my attention almost immediately that Venezuela was growing in importance as a command and control hub,” he says. “The traffickers could operate there with impunity, partly because we had limited visibility there after Chavez shut down the DEA.” Maltz also feels that Europe should be grateful for the US’ action despite the unease from some leaders, including Sir Keir Starmer, over the legality of the operation.
“The Venezuelans have been weaponising drugs to harm Americans, and inundating Europe with cocaine too – I don’t think Europeans quite realise how much of a major player Venezuela has become in the drug trade,” Maltz says. “President Trump isn’t [only] helping keep America free of this trade, he’s helping Europe too.”
Source: www.drugwatch.org































































































The Princess of Wales is patron of The Forward Trust, a charity devoted to assisting addicts to remain abstinent from their drug of addiction. She has just spoken out forcefully against the view that addiction is weakness of will or any kind of moral problem.
“Addiction is not a choice or a personal failing,” she said, implying thereby that it was a medical condition like any other, such as Parkinson’s disease or multiple sclerosis. She said that “people’s experience of addiction in still shaped by fear, shame and judgment, and that this ought to change”.
I am sure that HRH meant well, and that she feels genuine sympathy for addicts; but unfortunately, her view is simple, unsophisticated, dehumanising and empirically false.
It is dehumanising because, by denying that addiction is a choice, it deprives addicts of their agency both in theory and to a certain extent in practice. If, after all, you persuade someone that he does not make a choice in doing something, you also persuade him that choice cannot prevent him from doing it. He is not a human being like you and me, but a helpless feather on the wind of circumstance.
This turns him into an object, not a subject, both to himself and others. Such a view is implicitly degrading, demeaning and far from compassionate. It implies the need for an apparatus of care to look after him, much as one would look after an animal in a menagerie, with kindness but not with much respect.
Take the case of the injecting heroin addict and think what he has to do and learn to become such an addict. He has to learn where to obtain heroin and how to prepare it. He has to learn to disregard its unpleasant side effects. He has to overcome a natural aversion to pushing a needle into himself. This is not something that just happens to him.
Moreover, not only do most addicts take the drug for some time before becoming physically addicted to it, but they are fully aware in advance of the consequences of taking the drug long-term. Addicts are not “hooked” by heroin, as they often put it; rather, they hook heroin.
It is untrue that addicts require a professional apparatus to overcome their addiction. Millions of people have given up smoking, though nicotine is addictive. During the Vietnam War, thousands of American soldiers addicted themselves to heroin and gave up, with almost no assistance, one they returned home.
In 1980, Porter and Jick pointed out that people treated with strong painkillers as in-patients in hospital did not go on to become addicts once they left hospital. This was unfortunately interpreted to mean that such drugs were not addictive; but, on the contrary, it shows that addiction, in the sense of continuing addictive behaviour, is not straightforwardly a physiological condition.
At the root of the Princess’s misapprehension is the post-religious or secular view that if a person is the author of his own downfall, he is due no sympathy or compassion. It is a highly puritanical view, and since we do not want to be puritans, we make the problem a medical one instead. But since we are all sinners and the authors of our own downfall, at least in some respect or other, this also has the corollary that sympathy or compassion is due to no one when he needs it.
The Princess appears to think that if you say to an addict that he has behaved, and continues to behave, foolishly and badly, you are necessarily saying to him, “Go away, darken my doors no more”. She seems to think that the truth, far from setting people free, will imprison them until someone comes along with a technical key to unlock them.
Of course, some addicts benefit from assistance, but not for the reasons the Princess supposes. Medication may reduce their physical sufferings, and if we take once more the example of injecting heroin addicts, we discover that they may well have so destroyed their relations with everyone – their families and friends – that there is no one to whom to turn if they desire to change their ways. They thus need a helping hand, but this is not the same as removing fear or stigma (a very necessary, though not sufficient, aid to civilised life). Though she did not mean them to be so, the Princess’s words were not so much demoralising, as amoralising.
Source: https://www.telegraph.co.uk/gift/51db8fdbd5d80cb6